History
A 62-year-old woman was seen at the cardiology outpatient clinic. Her medical history was significant for the onset of mild heart failure symptoms 2 years previously. She had a past left ventricular ejection fraction (LVEF) of 32% and a diagnosis of nonischemic cardiomyopathy because no significant coronary artery disease was seen on coronary angiography. She was treated medically for heart failure and had undergone implantable cardioverter-defibrillator (ICD) placement. Because she did not have a left bundle branch block (LBBB), she was not considered for cardiac resynchronization therapy (CRT) at the time, with New York Heart Association (NYHA) class II heart failure symptoms. She remained active, working full time, but recently had 6 months of progressive dyspnea on mild exertion, consistent with NYHA class III heart failure symptoms. She was treated with loop diuretics, an angiotensin-converting enzyme inhibitor, and carvidilol. Her medical history is significant for hysterectomy, oophorectomy, appendectomy, tonsillectomy, and mild hypothyroidism. She previously smoked one pack of cigarettes per day but quit smoking 11 years ago.
Comments
This patient has nonischemic cardiomyopathy with an ICD implanted as a primary prevention indication. She experienced 6 months of progressive dyspnea on exertion.
Current Medications
The patient was taking furosemide 40 mg daily, enalapril 10 mg twice daily, carvedilol 12.5 mg twice daily, atorvastatin 10 mg daily, levothyroxine 25 mcg daily, and aspirin 325 mg daily.
Comments
This patient was on appropriate pharmacologic therapy for systolic heart failure.
Current Symptoms
The patient was experiencing progressive dyspnea that occurred with everyday activity and occasional ankle swelling. She denied chest pain, paroxysmal nocturnal dyspnea, palpitations, lightheadedness, or syncope.
Comments
These symptoms are consistent with heart failure, in NYHA class III. She was referred for echocardiography and consideration for CRT.
Physical Examination
Comments
Mild ankle edema supports the diagnosis of heart failure. Systolic murmur at the left sternal border is consistent with known mild tricuspid regurgitation.
Laboratory Data
Comments
No laboratory abnormalities were present that would account for worsening heart failure.
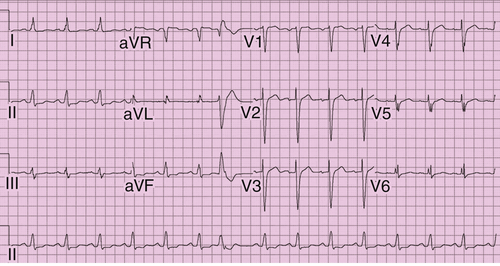
Electrocardiogram
Findings
The electrocardiogram (ECG) revealed normal sinus rhythm, occasional premature ventricular complexes, nonspecific intraventricular conduction delay with a QRS width of 140 ms, and nonspecific T-wave changes (Figure 36-1)
Comments
The patient has a widened QRS complex with a duration greater than 120 ms. However, the morphology of the QRS complex is not a typical LBBB and the QRS duration is intermediately widened (range 120-149 ms).
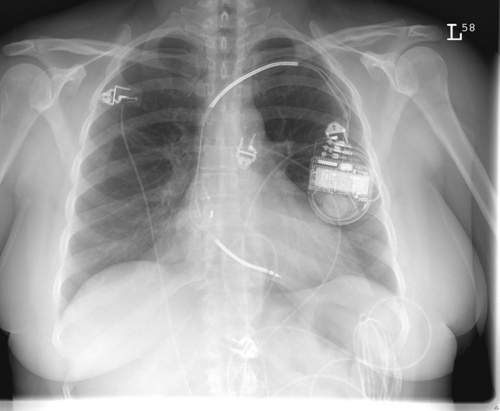
Chest Radiograph
Findings
The chest radiograph showed cardiomegaly with past ICD implantation and evidence of pulmonary vascular congestion (Figure 36-2).
Comments
Evidence of mild congestive heart failure was confirmed on radiography.
 Echocardiogram
Echocardiogram



