Figure 32.2 The flexible tube of the endoscope. Reproduced with kind permission from Imotech medical, formerly Fujinon.
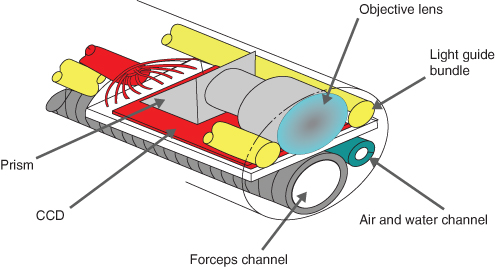
Figure 32.3 The accessory or biopsy channel. Reproduced with kind permission from Imotech medical, formerly Fujinon.
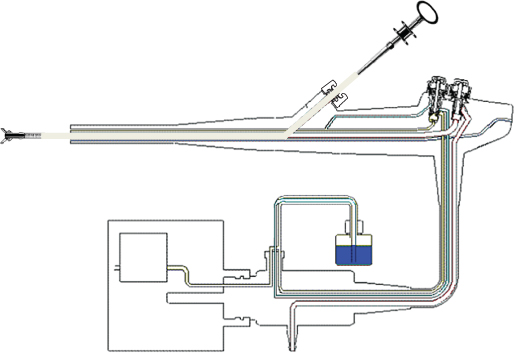
Figure 32.4 The suction channel. Reproduced with kind permission from Imotech medical, formerly Fujinon.
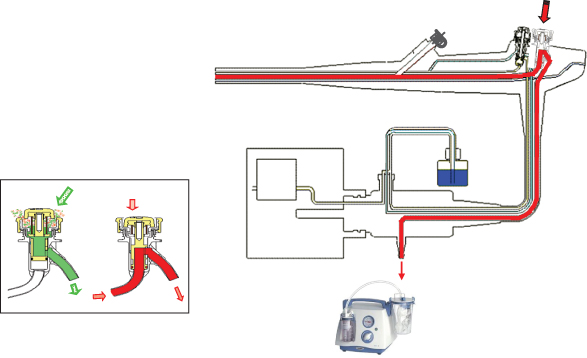
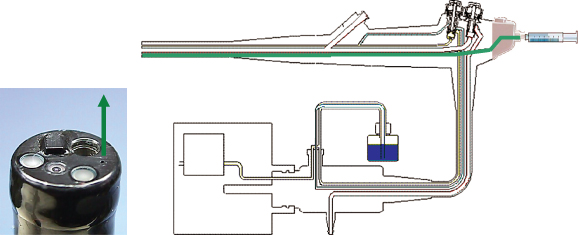
Figure 32.5 The air (a) and water (b) channels. Reproduced with kind permission from Imotech medical, formerly Fujinon.
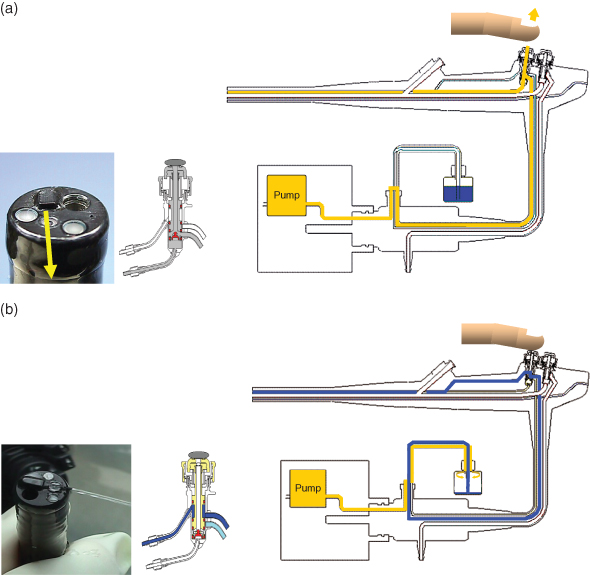
Figure 32.6 The jet channel. Reproduced with kind permission from Imotech medical, formerly Fujinon.
Preparation of the Endoscopy Room
Preparation involves the accumulation of the necessary equipment and checks to ensure it is fully functional, clean and safe to use. The equipment required for an endoscopy will vary according to the type of endoscopy requested and the clinical indication.
The endoscope will need to be processed in an automatic endoscope reprocessor (AER) and used within 3 hours. Processed endoscopes can be stored in an endoscope storage cabinet for a maximum of 72 hours prior to use.
Setting up the Procedure Room
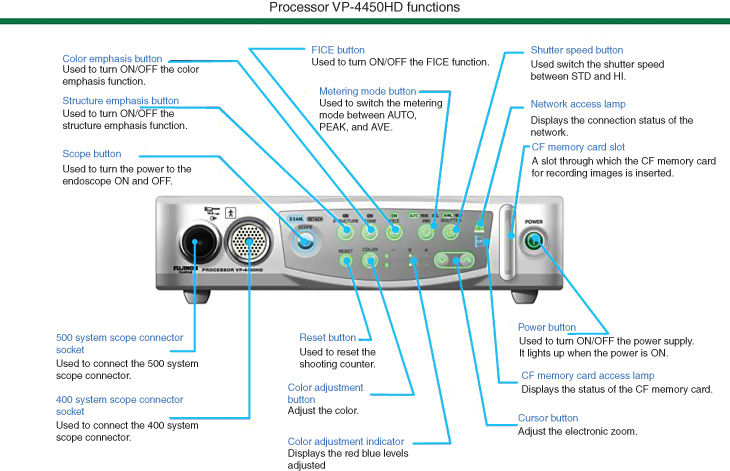
The endoscope is connected directly to a light source (Figure 32.7) and processor (Figure 32.8) which carries the image from the endoscope to a screen. The screen enables the whole team to view the upper or lower gastrointestinal tract.
The endoscope processor and light source are stored on a purpose-built trolley that also acts as a working space for the endoscopy assistant on which can be placed a container of water to test the correct functioning of the endoscope, swabs, mouth guard for gastroscopy, lubricant, specimen containers and a syringe for flushing the endoscope and cleaning the endoscope lens.
Supplementary Equipment
A supply of single-use sterile equipment should be readily available and placed either in the procedure room or in an adjacent area such as:
- biopsy forceps for taking tissue samples
- snares for removing and cauterising (diathermy) polyps
- hot biopsy forceps to cauterise small polyps
- dilation balloons for expanding strictures
- clipping apparatus for control of bleeding points
- injection needles for injecting sclerosing agents, tattooing lesions and lifting polyps to enable a better clearance margin and to reduce the possibility of perforating the colon
- plus a diathermy machine.
Sengstaken tubes must be available for emergency procedures, where control of oesophageal variceal bleeds may not be possible endoscopically.
Figure 32.7 Example of light source functions. Reproduced with kind permission from Imotech medical, formerly Fujinon.
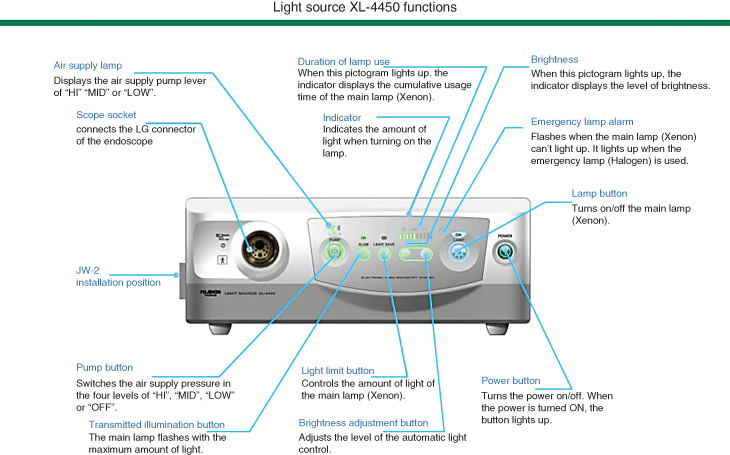
Figure 32.8 Example of processor functions. Reproduced with kind permission from Imotech medical, formerly Fujinon.
Suction
Suction apparatus is required to remove the patient’s secretions orally and also via the endoscope, for this reason two independent suction sources need to be available as well as in an emergency setting, where a patient is bleeding profusely, a second patient suction unit is needed as one may not manage the blood flow and maintain a clear patent airway.
Oxygen
Oxygen administration via nasal prongs, nasal catheter or face mask is required either through wall-mounted access points or via a cylinder, as oxygen saturation levels may drop during the endoscopy and recovery period, whether the patient is sedated or unsedated, especially if an opioid has also been administered.
Monitoring
Patient monitoring equipment must be available to measure the pulse, blood pressure, oxygen saturation levels and respiratory rate, which need to be recorded on the care plan along with consciousness levels and pain scores.
The procedure may be performed under sedation, using a topical local anaesthetic spray to numb the patient’s throat if not having sedation, or, in an emergency setting, under a general anaesthetic.
Medication
The medications available to the endoscopist will include a sedative such as midazolam, lignocaine throat spray, opioid analgesia for colonoscopy or painful procedures and reversal agents for the sedation and opioid mediations such as flumazenil and naloxone. Nitrous oxide and oxygen (Entonox) is useful for painful procedures, especially in patients who are not well enough to be prescribed sedation or opioid medications. It is also an excellent alternative to sedation and/or opioid medications for day-case patients as the effects are dissipated within 30 minutes of cessation of administration, enabling patients to drive their vehicle from the hospital and return to normal activities without a prolonged recovery period.
Sclerosing agents, such as adrenaline, may be injected into bleeding points within the gastrointestinal tract such as gastric and duodenal ulcers to control bleeding.
Buscopan may be required to relax smooth muscle and reduce spasm within the gut, thus aiding clearer views of the cavity.
Resuscitation
All clinical areas must have resuscitation drugs and equipment. The resuscitation equipment should be latex free and, where appropriate, single use.
In addition to the basic monitoring equipment there must be provision of equipment for the airway and circulation, resuscitation drugs, a defibrillator and stethoscopes. A 12-lead ECG and a blood gas analyser should be available.
Clinical areas should have immediate access to stethoscopes, a device for measuring blood pressure, a pulse oximeter, a 12-lead ECG recorder and facilities for blood gas analysis (Resuscitation Council 2004).
Intravenous fluids may be required, especially for patients who have been nil-by-mouth for long periods or who have taken bowel cleansing preparation as they may become dehydrated. Emergency patients may require colloids (e.g. Gelofusine) or blood transfusion if bleeding.
Photography
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


