History
An 81-year-old patient with type 2 diabetes and hypertension as cardiovascular risk factors sought treatment because of effort-related dyspnea (New York Heart Association [NYHA] class III) and presyncopal episodes. A complete cardiologic assessment was performed. On the baseline electrogram (ECG), atrial fibrillation with incomplete left bundle branch block (LBBB) was found; at transthoracic echocardiography, dilatative cardiomyopathy with reduced left ventricular ejection fraction (LVEF 25%) was the main finding, together with a moderate left atrial dilation (anteroposterior diameter 51 mm) and moderate mitral regurgitation. A 24-hour Holter ECG recording also was performed that evidenced atrial fibrillation with a mean ventricular rate of 90 bpm and no pathologic pauses. Medical therapy was optimized, but in a few months no improvement was observed. The patient therefore received a biventricular implanted cardioverter-defibrillator (ICD) (no atrial lead was implanted because atrial fibrillation was considered permanent).
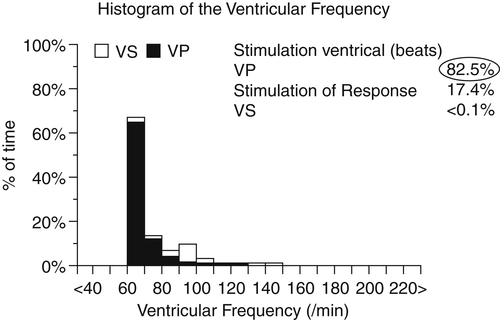
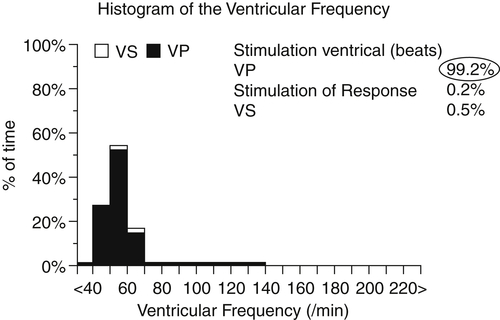
Six months later, LVEF was slightly improved (30%) and no changes were found in left atrial dimension and mitral regurgitation. Electronic device control also was done, and a suboptimal biventricular pacing percentage was found (82%, Figure 31-1) because of the high rate of atrial fibrillation with spontaneous atrioventricular conduction. No clinical changes were observed. These findings were considered secondary to lack of biventricular full-time pacing, and the patient underwent atrioventricular junction ablation. After 3 months of full-time biventricular stimulation (Figure 31-2), further improvement in LVEF was observed (from 30% to 40%), along with mitral regurgitation and left atrial diameter reduction. The patient reported clinical improvement (no further presyncopal episodes, NYHA class IIB). Surprisingly, at baseline ECG, regular sinus activity was found. The issue was whether to proceed with system upgrade by atrial lead implantation.
Comments
After ICD implantation, only slight instrumental benefit was observed without any clinical improvement. This was due to suboptimal biventricular pacing percentage, because biventricular devices are known to need almost full-time pacing to be effective. We therefore decided to perform atrioventricular node ablation, following which approximately 100% of biventricular pacing was obtained. The positive left ventricular remodeling induced by pacing led to an initial improvement in LVEF and the patient’s symptoms. Improving cardiac contractility and ventricular output, thus reducing filling pressure, may have played an important role in reducing atrial stretching, atrial pressure, and, subsequently, left atrial dimensions, removing one of the principal causes of atrial fibrillation. Moreover, mitral regurgitation was reduced as a result of resynchronization therapy. These may be the reasons why sinus rhythm was restored.
Current Medications
The patient was taking carvedilol 9.375 mg twice daily, furosemide 25 mg once daily, warfarin 5 mg based on international normalized ratio values, ramipril 5 mg once daily, digoxin 0.125 mg once daily, and amiodarone 200 mg once daily.
Comments
The patient was taking optimal medical therapy for heart failure; an angiotensin-converting enzyme inhibitor and a beta blocker were not fully titrated because of low blood pressure values. Amiodarone was administered even though atrial fibrillation was thought to be permanent as a rate control drug, because carvedilol and digoxin together were not enough. Of course, warfarin also was administered.
Current Symptoms
The patient was in NYHA class IIB, showing improvement after atrioventricular node ablation. Nevertheless, moderate effort-related dyspnea persisted. Despite advanced age, the patient normally engaged in moderate physical activity.
Comments
Improved cardiac contractility, left ventricular reverse remodeling, and reduced filling pressure provided by biventricular pacing, in the presence of optimal medical therapy and after atrioventricular node ablation, led to a better functional class. However, lack of atrial contractility resulting primarily from atrial fibrillation and then desynchronized atrial and ventricular activities once sinus rhythm was restored may have contributed to symptoms patient still reported.
Physical Examination
Comments
Even in the presence of a desynchronized atrial activity, no signs of congestive heart failure were found, thanks to biventricular pacing–induced improvements. Auscultatory findings related to mitral regurgitation were present.



