History
In 2002 the patient was diagnosed with Global Initiative for Chronic Obstructive Lung Disease stage II chronic obstructive pulmonary disease and in 2004 with first-degree atrioventricular block. In June 2011 he was admitted for decompensated heart failure. Echocardiography revealed a mildly dilated left ventricle, left ventricular ejection fraction (LVEF) of 20%, and grade III mitral regurgitation. Coronary angiography showed no significant coronary artery disease. Frequent premature ventricular contractions were observed during admission. Medical therapy for heart failure was initiated, and the patient was scheduled for reevaluation.
In October 2011 frequent premature ventricular contractions were reported on a 24-hour Holter monitor (28% of all QRS complexes, with one dominant morphology accounting for 99% of all premature ventricular contractions). Drug therapy with metoprolol 75 mg twice daily was not effective, sotalol was not tolerated, and metoprolol was continued.
In December 2011 the patient was readmitted for intermittent total atrioventricular block reported on a 24-hour Holter monitor. He was in New York Heart Association (NYHA) class III. On an echocardiogram, LVEF was 30%, with grade I to II mitral regurgitation. Despite discontinuation of metoprolol therapy, the total atrioventricular block became permanent. A temporary pacemaker was inserted, followed by cardiac resynchronization therapy defibrillator (CRT-D) implantation.
Current Medications
The patient was taking calcium carbasalate (Ascal) 100 mg daily, spironolactone 12.5 mg daily, simvastatin 40 mg daily, perindopril 4 mg daily, furosemide 40 mg daily, and metoprolol 50 mg twice daily.
Current Symptoms
The patient had marked limitation of physical activity (NYHA class III), with no chest pain or collapse.
Physical Examination
Laboratory Data
Electrocardiogram
Findings
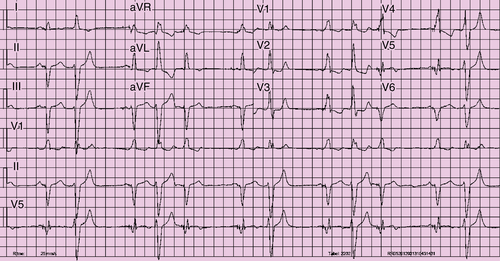
An electrocardiogram revealed biventricular pacing with frequent premature ventricular contractions and QRS during biventricular pacing at 160 ms (Figure 27-1). Premature ventricular contractions occurred with slightly varying morphology, all right bundle branch block (RBBB) type of morphology (defined as dominant R in precordial lead V1), left superior axis, transition V4-5.
Echocardiogram
Findings
An echocardiogram showed a dilated left ventricle, no hypertrophy, and an LVEF of 41%, with akinesia of the basal inferolateral wall, no left ventricular thrombus, and grade I to II mitral regurgitation, with eccentric jet along the lateral wall of the left atrium. The mechanism is likely restriction of the posterior mitral leaflet.
Physiologic Tracings
Findings
The 24-hour Holter monitor showed sinus rhythm with biventricular pacing, and frequent premature ventricular contractions (33% of all QRS complexes) were seen, 96% of which were monomorphic.
Focused Clinical Questions and Discussion Points
Question
When the patient developed total atrioventricular block in December 2011, did he need biventricular pacing or would right ventricular pacing have been sufficient?
Discussion
In December 2011 the patient had marked limitation of physical activity (NYHA class III), impaired left ventricular function (LVEF 30%), grade I to II mitral valve regurgitation, and an indication for permanent ventricular pacing because of total atrioventricular block. Several studies have demonstrated the deleterious effects of chronic right ventricular pacing, which include intraventricular and interventricular mechanical dyssynchrony, ventricular dilation, and decreased LVEF. Also, right ventricular pacing may further aggravate mitral valve regurgitation,1 which was already grade I to II at that stage, despite drug therapy. The deleterious effects on left ventricular function may be particularly important in patients who already have left ventricular dysfunction. The Homburg Biventricular Pacing Evaluation (HOBIPACE) trial was the first study to compare biventricular pacing to right ventricular pacing in patients with reduced left ventricular function and a standard indication for permanent ventricular pacing.5 Using a cross-over design, 30 patients received 3 months of right ventricular pacing and 3 months of biventricular pacing. In contrast to right ventricular pacing, biventricular pacing resulted in smaller left ventricular end-diastolic and end-systolic volumes, a higher LVEF, lower N-terminal prohormone of brain natriuretic peptide concentrations, higher maximum exercise capacity, and better quality of life. According to the current guidelines for cardiac pacing and CRT,6 CRT may be considered in patients with reduced LVEF who require chronic pacing and in whom frequent ventricular pacing is expected. However, the evidence for this approach is limited, as indicated by the class C recommendation.