From Royal College of Anaesthetists (2009), British Anaesthetic and Recovery Nursing Association (2005) and ASPAN (2010a).
The evidence supporting PACU staffing numbers is limited and in the majority of incidences, relates to ‘expert opinion’ and ‘best guess’ scenarios. The PACU is an unpredictable environment that is further complicated with the delays in discharging patients back to the ward or critical care facility. These delays can impact on the ability of the department to admit new patients, causing a bottleneck and slowing the patient pathway through theatre (Smedley 2010). It is essential to keep the patient pathway through theatre, recovery and return to the ward as smooth as possible to avoid bottlenecks and delays. The key to this smooth running is communication between areas and an understanding of each others’ needs and issues and ensuring that the patient’s safety is the fundamental issue.
Daily Equipment Checking
All bedside equipment should be checked prior to the patient’s arrival in recovery. Checks should include the following:
- Oxygen flow should be checked by switching the oxygen on and ensuring there is uninterrupted flow.
- Suction should be checked to ensure that it maintains and increases pressure when the tubing is kinked or suctioning fluids.
- Bedside emergency ventilation equipment should be tested to ensure that there are no leaks in the bag or obstructions in the oxygen flow.
- Equipment should be changed as each patient is discharged, and the area and non-disposable equipment wiped down as per hospital infection prevention and control policies.
All emergency equipment should be checked on a daily basis or as per the department schedule to ensure that it is in full working order. When the equipment is used, it must be replaced as soon as possible so that it is ready for next use.
Patient Transfer from Theatre to PACU/Handover of Patient
The patient will be accompanied to the PACU by the anaesthetist and an operating room practitioner. Oxygen is delivered en route and must be attached to wall delivery on arrival in PACU. The patient should be received by two PACU practitioners to ensure safe transfer of care, management of monitoring systems, intravenous infusions, drains and urine bags (BARNA 2005). Handover will include patient name, relevant medical history, anaesthetic technique and drugs, intraoperative complications and operative detail including sutures, dressing and drains. Instructions for postoperative care from both surgeon and anaesthetist are detailed at this time. At this point the PACU practitioner will rapidly assess the patient in order of clinical priority of airway, breathing and circulation. The anaesthetist should remain to assess that the patient is breathing spontaneously and the PACU practitioner is ready to take over care (AAGBI 2002). Clinical guidelines may be given based on patient’s baseline observations, anaesthetic and surgical history. Documentation is completed as soon as the patient is stable.
Risk Assessment of Patient in Planning Care
The patient undergoes dynamic physiological changes in this initial postoperative period due to the profound impact of anaesthesia and surgery on normal body function as illustrated in Table 23.2. Planning patient care follows risk assessment in order to evaluate potential complications associated with the patient’s medical history, surgical and anaesthetic process. The PACU practitioner will gather information both from anaesthetic/theatre handover, together with use of the anaesthetic record and surgeon’s notes.
While risk assessment alerts the practitioner to potential complications, it is by rigorous continual physical assessment of all body systems followed by rapid intervention and reassessment that safe patient outcomes are achieved. Baseline recordings of airway patency, respirations, blood pressure, level of consciousness, core temperature, sedation/pain and nausea scoring are noted. Monitoring of pulse oximetry, electrocardiogram and the use of non-invasive blood pressure are now routine (AAGBI 2007). Central venous pressure, arterial blood gas results may be used dependent on the complexity of the procedure and patient medical history. Capnography is recommended by the AAGBI (2009) for all intubated patients and those whose airway is maintained by supraglottic or other similar airway devices.
Table 23.2 Anaesthetic and surgical risk factors.
| Anaesthetic/surgical process | Risk of complications in PACU |
| Induction agents Induce unconscious state Airway maintenance: laryngeal mask airway, endotracheal intubation Maintenance agents Maintain unconscious state Reversal agents Reverse muscle relaxant (neostigmine) Hypothermia Fluid loss Pain | Propofol may leave mild hypotension Intubation potentiates risk of laryngospasm Opioids, failure to wake, respiratory depression, airway obstruction Volatile anaesthetic agents, failure to wake, respiratory depression, vasodilation and hypotension, airway obstruction Muscle relaxants, residual respiratory muscle weakness, residual paralysis if not reversed, airway obstruction Inadequate dose of neostigmine results in residual paralysis Mild to profound hypothermia delays recovery Clear fluid/blood loss – will result in circulatory disturbance Pain causes distress and stimulation of sympathetic nervous system – tachycardia and potential cardiac stress |
Intraoperative fluid balance is noted, taking into consideration actual drainage into urinary catheter bags and drains. Observations are routinely noted every 10 minutes while the patient is in the PACU. The early stages of patient recovery are when the patient is most vulnerable to sudden clinical changes. While progression towards full recovery and homeostasis is the norm, at any stage the patient’s condition may deteriorate and complications set in.
Airway: the First Priority
Multiple anaesthetic agents as shown in Table 23.2 can lead to delayed return to consciousness with loss of normal airway protective mechanisms (swallow, cough and gag reflexes) combined with upper airway muscle weakness. The delicate structures of the upper airway function normally to allow the free passage of air to and from the lungs.
Upper airway structures
The tongue is a large muscular organ which helps in the mastication of food before swallowing. The adult pharynx is a 13-cm-long muscular channel comprising the nasopharynx, oropharynx (throat) and hypopharynx, communicating with the oesophagus and larynx (Figure 23.1). Food and water pass via the oropharynx and, on swallowing, are diverted to the oesophagus, which lies posterior to the trachea en route to the stomach. The epiglottis (a leaf-like cartilage) folds over the vocal cords on swallowing to ensure that food does not pass into the trachea. The vocal cords are narrow ligaments contained in the larynx which allow speech and the free flow of air to the lungs.
From the induction of anaesthesia until the patient is awake (with the return of muscle tone and vital reflexes) these structures are at risk of malfunction, leading quickly to airway obstruction (Table 23.3).
Airway assessment
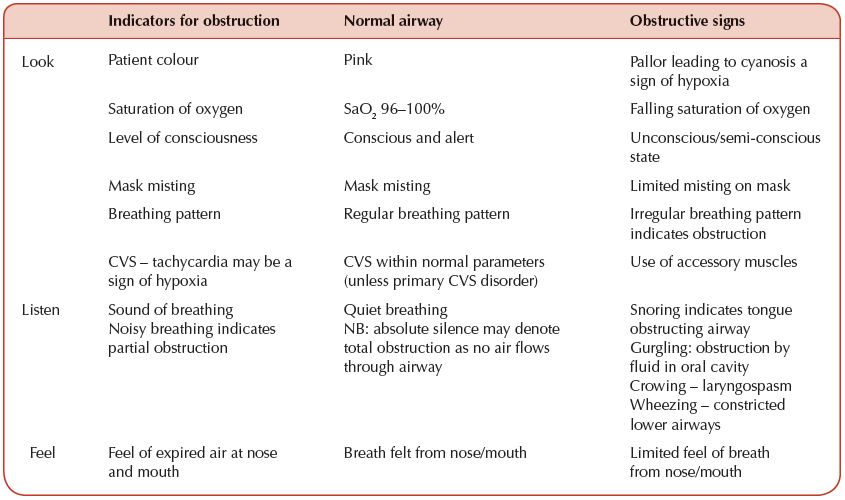
Airway obstruction in the immediate post-anaesthetic phase is a common and potentially dangerous complication in the semi- or unconscious patient whose protective reflexes have not returned. Risk factors for obstruction should be assessed in planning care. Use of narcotics, muscle relaxants, surgical procedures and obesity may all cause obstruction. Complications are avoided by rigorous continuous physical assessment, recognition of early derangement from the norm and rapid appropriate intervention. The PACU practitioner uses the ‘look, listen, feel’ method to comprehensively assess the airway as in Table 23.4.
Airway management
Airway management may be considered in three stages commencing with the use of routine manoeuvres to prevent or relieve obstruction.
Figure 23.1 The pharynx is a muscular channel comprising the nasopharynx, oropharynx and hypopharynx.
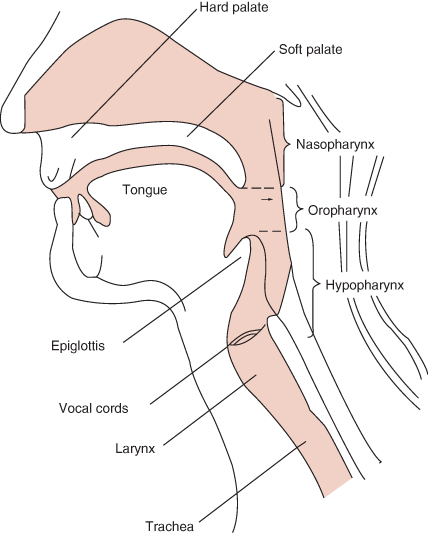
Table 23.3 Effect of general anaesthesia on normal airway function.
| Anatomical point | Surgery/anaesthetic risk | Potential for airway obstruction |
| Nasopharynx: nostrils | Ear, nose and throat (ENT) surgery: nasal intubation | Highly vascular area – bleeding may obstruct airway |
| Oropharynx: tongue/ oral cavity | Anaesthetic agents: muscle weakness ENT/dental surgery | Tongue floppy – falls to back of oropharynx Foreign body (throat/dental pack) blocks airway Bleeding from oral cavity/saliva |
| Laryngeal structures Epiglottis Vocal cords (glottis) | Anaesthetic agents relax the larynx leaving the airway unprotected Clumsy intubation causes risk of laryngospasm | Loss of epiglottal function: aspiration of food/fluid into trachea Partial or total obstruction caused by irritation to vocal cords |
Stage 1: Routine airway manoeuvres
A variety of techniques are used to ensure the airway remains clear. While unconscious, the tongue constitutes a major risk of obstruction. The laryngeal mask airway (LMA) left in situ is a valuable airway adjunct which prevents the tongue from occluding the oropharynx and should not be removed until the patient is waking and no longer able to tolerate it. The LMA may be withdrawn along with secretions if the cuff is left inflated where possible. If the LMA is not in situ and partial obstruction by the tongue is indicated by snoring, the use of the head tilt and chin lift may ease the obstruction. If this fails, jaw thrust manoeuvre is indicated (Figure 23.2). It may be necessary to insert a Guedel airway and if this fails to relieve obstruction the next step would often be reinsertion of LMA. Careful suctioning or placing the patient in recovery position, head down, can relieve obstruction by fluids in the oral cavity. Examination of the oropharynx will reveal obstruction by foreign body (tooth, dental pack). Oxygen is turned up to full flow if there is any sign of obstruction. Ongoing physical assessment confirms whether any of the above manoeuvres has successfully cured the obstruction. If clinical deterioration is seen, anaesthetic help must be sought immediately and an attempt to force oxygen into the airway by positive pressure bagging should be performed. If airway obstruction is sustained for many minutes brain death may follow.
Stage 2: Bagging patient using bag–valve–mask
It may require two practitioners to use the bag–valve–mask – one to hold the mask, the other to perform bagging while waiting for the anaesthetic team to take over management of this critical situation (Figure 23.3). With an oxygen reservoir bagging may open up the airway and deliver 96% O2. PACU staff must have the emergency intubation trolley ready with equipment and drugs that may be needed by the anaesthetist.
Figure 23.2 Jaw thrust. The mandible is pushed forward and lifts the tongue from the back of the oropharynx.

Stage 3: Patient intubation
If the above manoeuvres fail to remove the obstruction then endotracheal intubation will be necessary. It is often difficult in emergency situations to identify the prime cause of obstruction. Prior to intubating the patient the anaesthetist may try to alleviate the condition by administration of reversal drugs (neostigmine/naloxone/doxapram) (see Table 23.6). If the patient fails to respond then the role of the PACU team is to assist the anaesthetist in patient intubation.
Laryngospasm
Laryngospasm is the partial or complete spasm of laryngeal muscles preventing the free flow of air to and from the lungs. Clumsy intubation, secretions (blood/saliva) are common causes of spasm. A crowing noise is the classic sign of stridor, together with agitation, decreased oxygen saturation, use of accessory muscles and irregular breathing pattern if spasm severe. Laryngospasm must always be treated as a clinical emergency and anaesthetic help must be sought immediately. Spasm may worsen, leading to complete closure of the glottis and onset of severe hypoxia. Positive pressure ventilation with 100% oxygen should open up the cords and careful suction may relieve spasm caused by blood or secretions. Steroids, lignocaine or epinephrine may be used to decrease airway irritation. Failure to relieve spasm may require administration of muscle relaxants and re-intubation.
Aspiration
Aspiration of foreign body, blood or gastric contents into the lungs in the unprotected airway may occur while the patient is returning to full consciousness. Those at high risk include patients who are obese, pregnant or suffering from hiatus hernia. Coughing, bronchospasm, airway obstruction with resulting hypoxia may indicate aspiration. Any sign of aspirate dribbling from the mouth should be taken seriously and anaesthetic help summoned. The patient should be laid in the recovery position, head down to drain secretions, and suction applied. Airway maintenance and prevention of hypoxia are key management objectives. Potential damage to the lungs from food particles and acid secretions depends on the size and nature of aspirate. Further management includes a chest X-ray, possible use of antibiotics and/or steroids and the patient should be followed up in the high dependency area.
Breathing: the Second Priority
External respiration is the act of inhaling air into the lungs on inspiration and exhaling carbon dioxide on expiration via an unobstructed airway.
All body cells require a constant supply of oxygen to maintain normal cell function. Oxygen is consumed by the tissues in the process of internal respiration. Failure to deliver oxygen to the cells results in hypoxia and acidosis caused by anaerobic metabolism, both causing cell death. Carbon dioxide (CO2) must also be eliminated constantly. A build-up of CO2 in the blood causes acidosis. Normal acid level (pH) for cell function is 7.35–7.42. This narrow margin must be maintained for normal cell function. Patients routinely receive oxygen while in the PACU via a Hudson mask at 40% to ensure optimal oxygen levels in the blood. If the patient has lung disease a Venturi system is used which delivers a constant fixed percentage of oxygen appropriate for the patient’s condition.
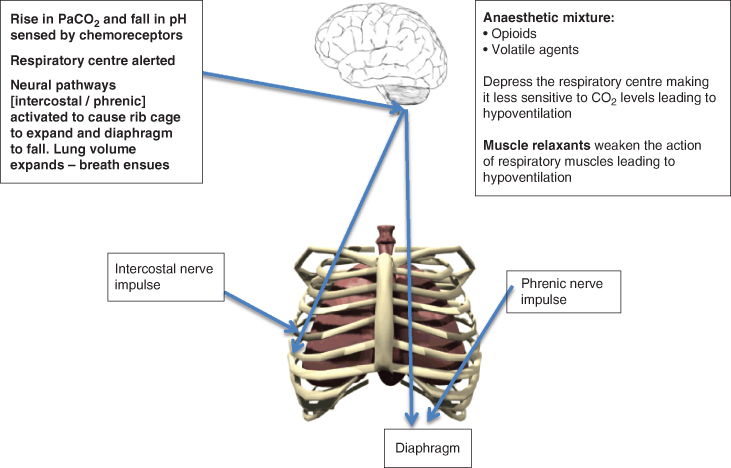
Control of breathing
The respiratory centre in the medulla of the brain is the control centre for breathing and stimulates inspiration (Figure 23.4). Peripheral chemoreceptors in the arteries sense rising levels of CO2 in the blood while central chemoreceptors monitor increased acidity of cerebral spinal fluid. The primary stimulus to breathe is to exhale carbon dioxide and maintain the pH level within its narrow margins. Oxygen lack, detected via the chemoreceptors, is a secondary stimulus to breathe.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree