CASE 23 Coronary Perforation
Cardiac catheterization
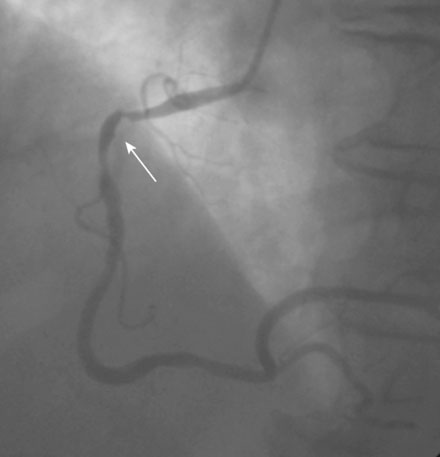
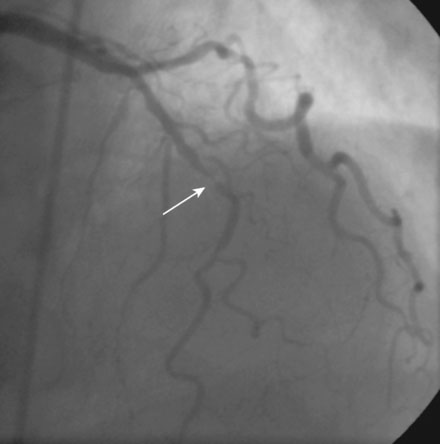
Coronary angiography revealed multivessel coronary disease with severe disease in the proximal segment of the right coronary artery and severe disease of the midportion of the left anterior descending coronary artery (Figures 23-1, 23-2 and Video 23-1). The operator judged the right coronary artery suitable for percutaneous coronary intervention; however, the left anterior descending artery provided several challenges. Not only did the vessel appear small in caliber, there was also marked tortuosity with diffuse disease surrounding the severely stenosed segment. Prior to the catheterization, the patient dismissed the option of bypass surgery and agreed only to percutaneous revascularization. The patient confirmed this after she was presented with the catheterization results, and the operator proceeded with a multivessel intervention on the right coronary artery and left anterior descending artery.