History
The patient has an extensive cardiac history, beginning with a myocardial infarction and subsequent coronary artery bypass and three grafts in 1988. In 2002, he underwent a reoperative three-vessel bypass. He was diagnosed with sick sinus syndrome in 2001 that required the implantation of a dual-chamber pacemaker. The device was updated to an implantable cardioversion defibrillator (ICD) in 2002 after he experienced cardiac arrest. He was successfully resuscitated without neurologic sequelae. The prior right ventricular lead was abandoned and capped, and the patient received a dual-coil high-voltage lead. The generator was replaced in 2005 and again in late 2011. On the current admission, the patient had poorly controlled hypertension and worsening heart failure in the setting of chronic right ventricular pacing. Left ventricular ejection fraction had fallen from greater than 55%, 1 year previously, to 31%. The patient experienced progressive dyspnea on exertion.
Current Medications
The patient was taking aspirin 81 mg daily, atorvastatin 80 mg daily, candesartan 16 mg daily, carvedilol 12.5 mg twice daily, dutasteride 0.5 mg daily, niacin 500 mg daily, and spironolactone 25 mg daily.
Physical Examination
Laboratory Data
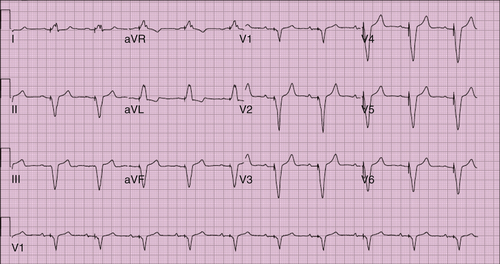
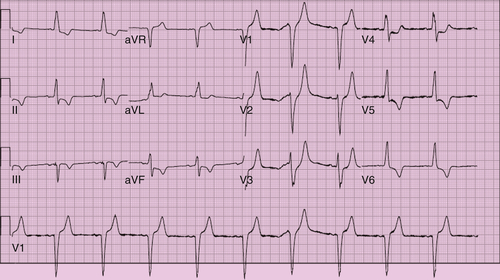
Electrocardiogram
Findings
The electrocardiogram revealed atrial-sensed ventricular-paced rhythm (Figure 21-1), with a heart rate of 62 bpm and QRS duration of 192 msec.
Sinus bradycardia with underlying left bundle branch block also was seen (Figure 21-2). The heart rate was 59 bpm and QRS duration 132 msec.
Atrial sensing and biventricular pacing were demonstrated on the electrogram (Figure 21-3), with a heart rate of 66 bpm and QRS duration of 138 msec.
Chest Radiograph
Findings
A frontal view of the chest demonstrates the heart to be normal in size and configuration (Figure 21-4). Median sternotomy sutures are present in the midline. A right-sided pocket is seen with an ICD and three leads: right atrial lead in the appendage, abandoned right ventricular pacing lead, and ICD lead in the right ventricular apex. The hilar and pulmonary vascular markings are normal, with no parenchymal infiltrates visualized.
The right ventricle appears normal in size and contractility (Figure 21-5). The intraventricular septum moves paradoxically toward the right in systole. The images demonstrate the left ventricle to be moderately dilated, with moderate diffuse hypokinesis. The left ventricular ejection fraction is 31%.
Computed Tomography
Findings
Computed tomography (Figure 21-6) with intravenous contrast was performed to visualize the status and location of previous grafts. The right atrial to left anterior descending, SV OM, and saphenous vein to right coronary artery grafts appear patent. The trajectory of the saphenous vein to obtuse margin graft was such that it allowed for consideration of placement of an epicardial lead on the basilar aspect of the posterolateral wall of the left ventricle. The proximal native coronary arteries are heavily calcified and occluded. There is mild cardiomegaly, with remodeling of the anterior wall of the left ventricle, presumably resulting from previous myocardial infarction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


