CASE 20 No-Reflow After Coronary Intervention
Cardiac catheterization
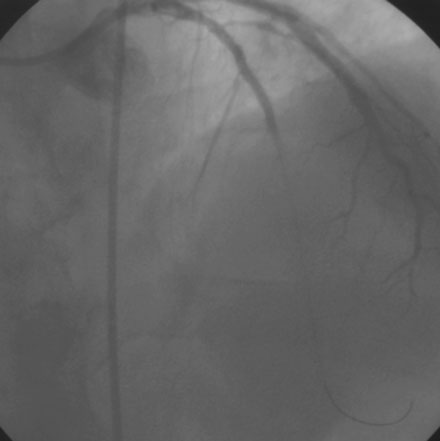
Diagnosed with a non-ST segment elevation acute myocardial infarction, he was admitted to a telemetry unit and treated with aspirin, enoxaparin, nitroglycerin, atorvastatin and metoprolol. He remained pain-free and underwent cardiac catheterization the following day. Left ventriculography was normal. Coronary angiography noted nonobstructive luminal irregularities in the right coronary and left circumflex arteries and severe narrowing in the proximal segment of the left anterior descending artery (Figure 20-1). Compared to the circumflex artery, angiographic flow appeared reduced at baseline (Video 20-1). After the intravenous administration of unfractionated heparin and eptifibatide, balloon angioplasty was performed using a 2.5 mm diameter by 20 mm long compliant balloon. Angiography performed after balloon dilatation showed complete occlusion of the left anterior descending artery at the site of the intervention (Video 20-2). The patient developed chest pressure but remained hemodynamically stable. An intracoronary bolus dose of 100 mcg of adenosine delivered through the guide catheter improved flow slightly; however, the entire artery did not fill with contrast (Video 20-3). There did not appear to be a dissection or other luminal problem responsible for the reduced flow, and the activated clotting time (ACT) was 280 seconds. The operator then deployed a tacrolimus-eluting stent (3.0 mm diameter by 28 mm long). Flow remained reduced, and the patient continued to experience chest pain after stenting despite repeated bolus injections of 100 mcg of adenosine (total of 500 mcg) injected through the guide catheter (Figure 20-2 and Video 20-4). At this point, the operator positioned an infusion catheter (Rapid Transit™ Catheter, Cordis Corporation) in the distal left anterior descending artery and injected an additional 100 μg adenosine. Subsequent angiography demonstrated nearly normal flow (Video 20-5) and the patient’s chest discomfort resolved.