There may be occasions when a patient-completed questionnaire will suffice in providing enough information about the patient’s health to determine that no further assessment is required before clearing the patient to be added to the waiting list. Such questionnaires can be completed in the outpatient department or the assessment clinic by the patient and handed in to a member of the nursing team, or patients may be asked the questions as part of a telephone assessment. These tend to be used for patients booked for minor procedures, or as a prescreening questionnaire to determine if/when a full assessment is required and with whom.
For patients due to undergo inpatient surgery, or who have very complex co-morbidities and are for day surgery admission, attendance at an assessment clinic for a face-to-face assessment may be appropriate.
Anticipation of equipment and documentary requirements for each patient should allow for a prepared area that allows the assessment to take place in privacy, giving respect to patient dignity and confidentiality. Interruptions should be kept to a minimum.
The patient may be asked to provide a urine sample to investigate for urinary tract infection, haematuria or glucosuria. If the department uses electronic assessment, then the patient will complete demographic information with the HCA or RGN. Observations will then be taken including regularity of pulse, blood pressure, respiratory rate and oxygen saturation levels. The height, weight and body mass index will be measured and documented. Swabs will be taken from nose, groin, catheter sites and any wound area to test for MRSA (methicillin-resistant Staphylococcus aureus) status (see External factors required at time of patient preparation point 1). For patients with respiratory disease, a peak flow measurement will be made and recorded. For those patients with a cardiovascular history or due for major surgery, an ECG may be required (NICE 2003).
With the above documentation, the RGN/FY1 will then have a range of information ready for his or her intervention.
History Taking
The RGN or FY1 will interview the patient in a private room, ensuring privacy and dignity. They should read through all available information provided, gaining clarity on specific issues before progressing to the discussion on the procedure itself.
Accurate history taking and recording is important and can be broken down into the following stages.
Accurate record of past medical, surgical, anaesthetic and social history
Attention to detail is important to enable a full understanding of a patient’s health or ill-health, co-morbidities, smoking or alcohol history. This will enable the assessor to gain insight into the past experiences of the patient, and to anticipate any potential areas that will require clarification or investigation. All records must at minimum be signed and dated and, if handwritten, be clear so as to avoid misinterpretation. Should a patient experience a clinical event (e.g. chest pain), it is important to record the time of the chest pain and its duration.
Complications from past medical, surgical or anaesthetic history
Unexpected outcomes and complications do occur and in order to minimise the chance of recurrence, it is important that the health professional has a clear understanding of what occurred, when and if possible why. This information allows the RGN/FYI to appropriately investigate potential causes/previously unknown health conditions, and thus optimise the condition prior to progressing with surgery. Investigations and resulting expert consultation with consultant and potential optimisation of the condition may delay the admission of the patient. The timing of the assessment should therefore be as early as possible in the surgical pathway.
Current symptoms/history
Having an understanding of the patient’s current symptoms will assist the health professionals to tailor the intervention appropriately. Information provided by the patient should be recorded in the clinical notes accurately and with clarity, ensuring date and time are entered, particularly when symptoms are changing. This information will be used by other health professionals and, in conjunction with the procedure and past medical history, form the base from which any improvements or deterioration of symptoms can be judged.
For patients due to have a general anaesthetic, questions should be asked relating to orthopnoea. This is because it is important to judge the patient’s ability to lay relatively flat for the length of the surgery without respiratory or cardiac distress. Questions could include the number of pillows a patient uses to sleep and if they sleep in a chair or bed and whether they suffer shortness of breath on exertion while climbing a flight of stairs or at night or at rest.
It is also useful to ascertain how far the patient can walk, and the reason why they stop, for example because of joint pain, dyspnoea, leg pains, chest pain, balance or fatigue. The response will lead the assessor to further questions and investigations.
Family history
Of particular note is immediate family incidence of reaction with anaesthetic, such as suxemethonium allergy or venous thromboembolism. These familial conditions are just two examples where the patient may have a predisposition and a full history and/or further testing may be required to reduce the risk of an untoward event.
Observations
Observations should be recorded during patient preparation and will form the baseline for changes in the observations during the perioperative period. The recorded results should be checked and any abnormal readings noted. It is good practice to repeat a raised blood pressure reading after 15–20 minutes.
Examination
The purpose of patient examination is to provide observation to accompany the history. Results will guide the assessor as to which investigations are required, if any, prior to reaching a decision as to the patient’s fitness to proceed with the surgery and/or anaesthetic.
Any pallor of the patient’s skin and signs of cyanosis, jaundice and anaemia should be observed, then checks made for oedema of the legs and sacrum, varicose veins, ulceration or pressure sores.
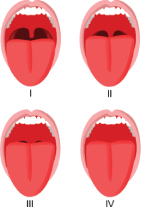
Checks on the patient’s neck flexion and extension should be carried out, and Mallampati Score checking used (Figure 2.2) for any restrictions which could cause difficulty with laryngoscopy or intubation (Mallampati et al. 1985, Nuckton et al. 2006).
Modified Mallampati Scoring is as follows:
- Class 1: Full visibility of tonsils, uvula and soft palate
- Class 2: Visibility of hard and soft palate, upper portion of tonsils and uvula
- Class 3: Soft and hard palate and base of the uvula are visible
- Class 4: Only hard palate visible.
The chest may also be examined. The trained professional should observe the position of the trachea, checking for any obstructions, the shape of the thorax noting any abnormalities that may indicate long-term respiratory disease. The patient should be asked about any cough or sputum, including the colour of any phlegm such as yellow or green indicating infection, or if the sputum is frothy, or blood streaked indicating haemoptysis. The chest is then palpated, checking for air entry to right and left side of the chest, before auscultation. Auscultation will provide the trained assessor with evidence of respiratory flow or restrictions – and is usually followed by cardiac auscultation, checking the heart valves for signs of regurgitation.
The venous thromboembolism risk assessment may be completed by the FY1 or RGN while the patient is in attendance for preparation. If completed at this stage then the form would need to be countersigned on admission (NICE 2010, Department of Health 2009).
Figure 2.2 Modified Mallampati Scoring is as follows: Class I: Full visibility of tonsils, uvula and soft palate. Class II: Visibility of hard and soft palate, upper portion of tonsils and uvula. Class III: Soft and hard palate and base of the uvula are visible. Class IV: Only hard palate visible. Reproduced from Wikimedia Commons – freely licensed media file. http://en.wikipedia.org/wiki/Mallampati.
Investigations
Routine investigations may be required for certain procedures according to local policy. History and examination will also prompt the assessor to request investigations to provide additional information prior to reaching a decision as to a patient’s fitness to proceed with the surgery and, if appropriate, anaesthetic. It is the responsibility of the assessor to check results of all investigations ordered and to take appropriate action on the findings.
Medication and Allergies
The pharmacist is key in patient preparation and several assessment clinics have pharmacist involvement. Where a pharmacist is not present then this role is undertaken by the RGN or FY1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


