History
The patient has dilated cardiomyopathy with an initial left ventricular ejection fraction (LVEF) of 25%, permanent atrial fibrillation (AF), and the cardiovascular risk factors of obesity (body mass index 32 kg/m²) and arterial hypertension.
The diagnosis of nonischemic dilated cardiomyopathy was established 1 year previously after angiographic exclusion of significant coronary artery disease, and medical heart failure therapy was initiated. Additionally, an antiarrhythmic treatment with amiodarone and an oral anticoagulation with phenprocoumon were initiated because of highly symptomatic paroxysmal AF mainly manifesting as debilitating palpitations. The amiodarone therapy, however, had to be terminated as a result of drug-induced hyperthyroidism after 3 months of treatment. Over the past several months, paroxysmal AF progressed to less symptomatic persistent AF, and after recent electrical cardioversion had failed to restore sinus rhythm, AF was considered permanent because the decision was made to cease further attempts of rhythm control interventions and to continue with a rate control strategy with metoprolol and digitoxin.2
The patient arrived for treatment with slowly progressive breathlessness, fatigue, marked limitation of physical activity corresponding to New York Heart Association (NYHA) functional class III, and ankle swelling despite optimal medical heart failure treatment. He also reports recurrent episodes of irregular heart action.
Current Medications
The patient’s current medications are metoprolol 95 mg twice daily; phenprocoumon with a target international normalized ratio of 2.5 (range 2.0 to 3.0); digitoxin 0.07 mg once daily; torasemide 10 mg twice daily; ramipril 10 mg once daily; and spironolactone 25 mg once daily.
Current Symptoms
The patient demonstrated progressive breathlessness, marked limitation of physical activity (NYHA functional class III), fatigue, severely reduced exercise capacity, mildly symptomatic irregular heart action, and recurrent ankle swelling. Anginal pain, dizziness, and syncopal events were denied.
Physical Examination
Laboratory Data
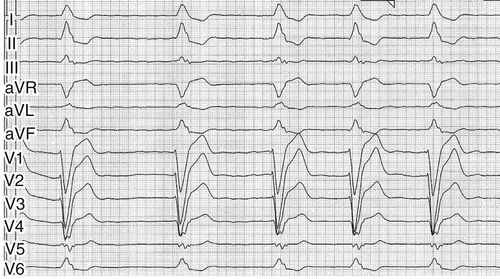
Electrocardiogram
Findings
The electrocardiogram recorded atrial fibrillation with a heart rate of about 55 bpm, normal QRS axis, left bundle branch block with a QRS duration of 150 ms, QT interval duration of 440 ms, and secondary repolarization abnormalities (Figure 2-1).
Chest Radiograph
Findings
The major radiograph findings on posteroanterior view were global cardiac enlargement, slight pleural effusions, and subtle pulmonary congestion (Figure 2-2).
Echocardiogram
Findings
Transthoracic 2-dimensional echocardiography revealed LV dilation (LV end-diastolic volume 222 mL, LV end-diastolic diameter 66 mm) and severe systolic dysfunction with a LVEF of 35% (Figure 2-3). Both the parasternal long-axis view and the 4-chamber view demonstrated a substantial dilation of the left atrium (50 mm in the parasternal long axis) (Figure 2-4). Clinically relevant valvular heart disease could be excluded.

Focused Clinical Questions and Discussion Points



