History
The patient had a complex past medical history. He underwent bioprosthetic aortic valve replacement in 2006 related to infective endocarditis with consequent severe aortic regurgitation and had moderately impaired left ventricular systolic function (left ventricular ejection fraction [LVEF] 45%-50%). Coronary angiography did not show significant coronary artery disease, and therefore surgical revascularization was not necessary at the time of aortic valve replacement.
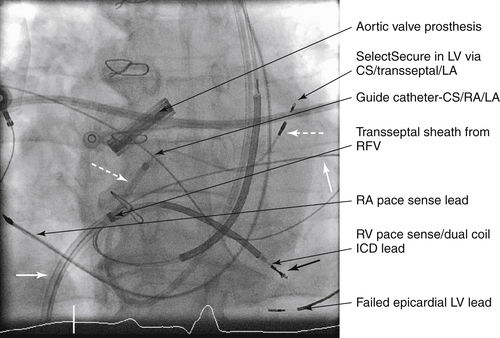
The patient then developed persistent (cardioversion on two occasions in 2007) and then permanent atrial fibrillation with fast ventricular rate response despite the use of digoxin, verapamil, and beta blockade (all in maximum tolerated or appropriate doses). He underwent atrioventricular nodal ablation in 2007 with implantation of a single-chamber rate-responsive right ventricular pacemaker.
Over the subsequent 2 years, he developed worsening systolic heart failure (New York Heart Association [NYHA] class III) that was refractory to medical therapy at maximal tolerated dosages (including an angiotensin-converting enzyme [ACE] inhibitor, beta blocker, nitrate, hydralazine, and loop diuretic). His ejection fraction was reduced to 35%. He therefore received an upgrade to a biventricular pacemaker.1 Because of the presence of an anomalous left-sided superior vena cava, left ventricular pacing via an epicardial coronary sinus branch was challenging. Nevertheless pacing was achieved at an anatomically appropriate site, although only one target coronary sinus tributary was available.
The patient responded well to biventricular pacing with improvement in ejection fraction (LVEF 45%) and NYHA status to class II.
Thirty-six months after implantation of the left ventricular pacing lead, he had late infection of the pacing pocket, with raised inflammatory markers and positive blood cultures for Staphylococcus.
Focused Clinical Questions and Discussion Points
Question
What is the indication for device and lead extraction?
Discussion
With evidence for both local and systemic infection, no other option is available but to perform system extraction.
Question
What is the reason for delay between extraction and re-implantation?
Discussion
This patient is pacing-dependent and requires temporary pacing before reimplantation of a new pacing system.
Question
What are the challenges of pacing via an anomalous left-sided superior vena cava draining into an enlarged coronary sinus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


