CASE 18 Unsuccessful Coronary Intervention
Cardiac catheterization
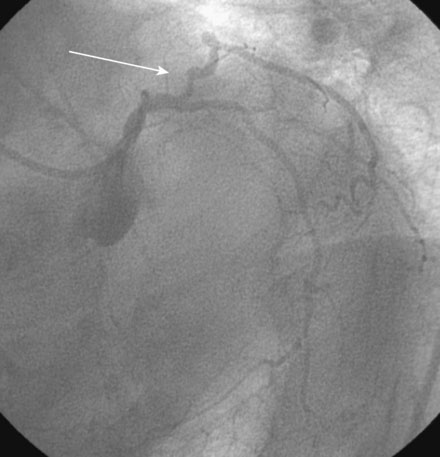
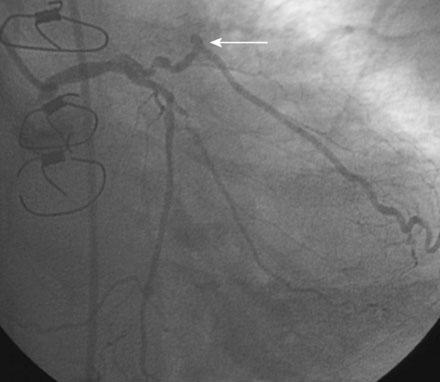
The diagnostic angiograms demonstrated occlusion of the native right coronary and left anterior descending coronary artery with occlusion of both saphenous vein grafts. A widely patent left internal mammary graft supplied a large left anterior descending artery. Severe disease of the proximal segment of a large first obtuse marginal artery as well as severe disease of a smaller-caliber second obtuse marginal artery likely accounted for her clinical presentation (Figures 18-1, 18-2 and Video 18-1). Based on these angiograms, stress test results, and her symptoms of progressive angina, her physician decided to revascularize the first obtuse marginal artery percutaneously.