History
The patient had a medical history of hypertrophic cardiomyopathy with progression to the dilated phase of cardiomyopathy (New York Heart Association class III) and conduction abnormalities, including a prolonged QRS duration of 154 msec with right bundle branch block (RBBB) and left anterior fascicular block. Her family history was positive for hypertrophic cardiomyopathy in her father and one brother. Genetic testing revealed a mutation in the TNNI3 gene, resulting in replacement of the normal glutamic acid codon with a glutamine codon at position 124 in the troponin I gene. She had no history of hypertension, dyslipidemia, diabetes mellitus, or tobacco use. An echocardiogram demonstrated an ejection fraction of 20% to 25%. She underwent attempted cardiac resynchronization therapy defibrillator (CRT-D) implantation at a different institution, but the coronary sinus could not be cannulated. In addition, concern existed about possible coronary sinus dissection. Therefore a CRT-D device was implanted, with the left ventricular lead port capped. The patient was referred for evaluation for potential upgrade to a CRT-D via the implantation of the left ventricular lead. Cardiac computed tomography angiography (CCTA) was ordered for further evaluation of anatomic abnormalities impeding coronary venous lead placement.
Current Medications
The patient was taking carvedilol 6.25 mg in the morning and 12.5 mg at night, enalapril 7.5 mg daily, spironolactone 25 mg daily, furosemide 10 mg daily, and potassium chloride 10 mEq daily.
Physical Examination
Laboratory Data
Comments
Renal insufficiency is a factor that must be taken into account with iodinated contrast studies, such as CCTA. This is an issue for the heart failure patient population who require CRT.
Electrocardiogram
Findings
The electrogram demonstrated an atrial paced rhythm and ventricular sensed rhythm at 60 bpm. The PR interval was 198 msec; QRS duration was 156 msec, with RBBB and left anterior fascicular block; and corrected QT interval was 450 msec. Left ventricular hypertrophy was present.
Echocardiogram
A transthoracic echocardiogram showed mild left ventricular enlargement with wall thickness at the upper limits of normal and severe global hypokinesis with akinesis of the midinferior wall, inferior septum, and apex. The left ventricular ejection fraction was 22%, with a left ventricular end-diastolic dimension of 54 mm, a posterior wall thickness of 11 mm, and an interventricular septal thickness of 12 mm. Mildly decreased right ventricular systolic function was noted, as well as biatrial enlargement, with a left atrial volume index of 43 mL/m2. The aortic valve was trileaflet, without aortic regurgitation or aortic stenosis. The mitral valve morphology was normal, with no evidence of mitral stenosis or regurgitation. No evidence of pulmonary regurgitation was seen. Trace tricuspid regurgitation was present, with an estimated right ventricular systolic pressure of 28 mm Hg. The right atrial pressure was estimated to be 5 mm Hg. The inferior vena cava size and respiratory variation were normal. No evidence of pericardial effusion was observed.
Cardiovascular Computed Tomographic Angiography
Findings
Coronary Venous Findings
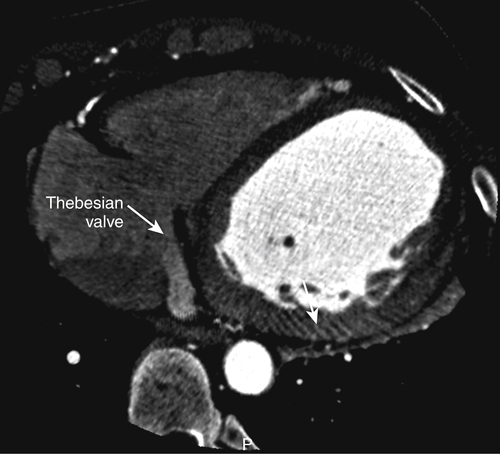
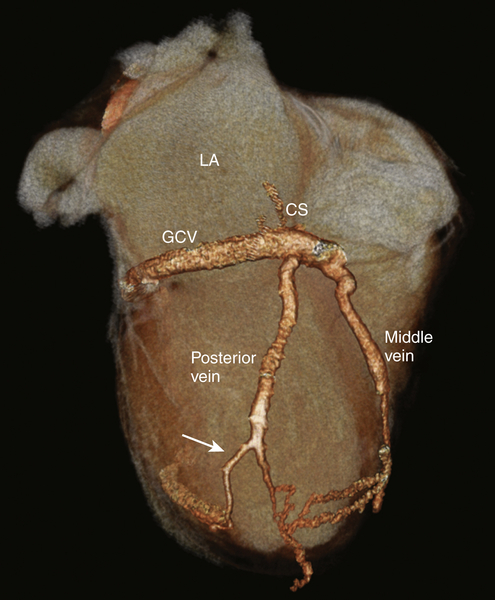
The coronary sinus ostium was patent, with an ostial diameter of 1.2 cm. A prominent Thebesian valve was noted covering the coronary sinus ostium (Figure 17-1). The middle cardiac vein was followed by a posterior cardiac vein branching off 1.5 cm after the coronary sinus ostium with a gentle angulation of 146 degrees and coursed posterolaterally (Figures 17-2 to 17-4). At 6 cm distal to the takeoff of the posterior vein (mid to apical ventricular level), the vein bifurcated, with one branch coursing posteriorly and the other laterally. No evidence of a branch vein in the lateral territory of the left ventricle was seen. An anterior interventricular vein was present. No evidence of coronary sinus dissection was noted.
Other Cardiovascular Findings
The coronary artery system was right dominant, with normal location of the coronary artery origins. Evidence of calcified and noncalcified plaques was present, without evidence of severe coronary artery stenosis (Figure 17-5). The left ventricle was moderately dilated, with thinning and aneurysmal dilation of the apex. A thin layer of mural thrombus was seen in the region of the apical aneurysm (Figure 17-6). The left atrium was severely enlarged. The right ventricle demonstrated normal morphology. The right atrium was normal in size. A dual-chamber implantable cardiac defibrillator (ICD) was present with leads in the right atrial appendage and right ventricular apex. The aorta and pulmonary arteries appeared unremarkable.