History
Nonischemic cardiomyopathy with a left ventricular ejection fraction of 15% to 20%, down from 30% in a span of 6 months, and New York Heart Association (NYHA) class III congestive systolic heart failure was diagnosed 5 months before the current admission. The patient also had a long history of chronic anemia that predates the decompensated heart failure. The patient was on optimal medical therapy. She underwent placement of an implantable cardioverter-defibrillator (ICD) 2 months earlier with the intent to place a cardiac resynchronization therapy device, but a left ventricular lead could not be placed through the coronary sinus. During the procedure, coronary sinus venography showed one high lateral branch with a proximal right-angle curve and a tight stenosis at the tip of the angle, a midcardiac vein with no posterior or lateral branches, and an anterior branch. The high lateral branch was cannulated with a Whisper wire, and using the over-the-wire technique an attempt was made to advance the lead into the branch. However, the lead could not be advanced beyond the stenosis. Repeat venography to better assess the severity of the stenosis demonstrated the vein to be occluded beyond the stenosis. Because no other vein suitable for transvenous left ventricular lead placement was available, the patient was referred for surgical epicardial lead implantation.
Current Medications
The patient was taking aspirin 81 mg daily, carvedilol 6.25 mg twice daily, furosemide 20 mg twice daily, potassium chloride 10 mEq daily, spironolactone 25 mg daily, and valsartan 40 mg daily.
Current Symptoms
The patient was experiencing shortness of breath when walking short distances (NYHA class III).
Physical Examination
Laboratory Data
Electrocardiogram
Findings
The findings on the electrocardiogram were ventricular rate 81 bpm, atrial rate 81 bpm, pulse rate 146 ms, QRS 140 ms, QT 420 ms, QTc 487 ms, and P-R-T axes 039, −51, and 127 degrees (Figure 16-1).
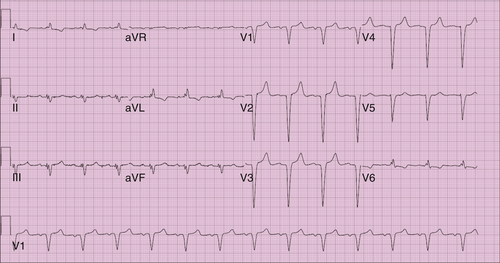
Comments
Normal sinus rhythm, left axis deviation, anterior wall myocardial infarction (age indeterminate) were noted.
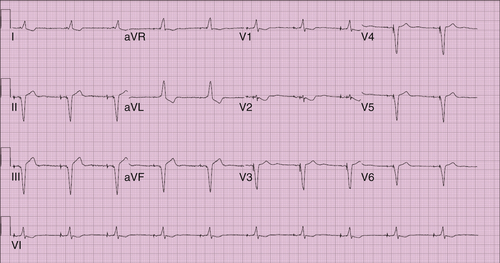
Findings
Repeat electrocardiogram findings were ventricular rate 60 bpm, atrial rate 60 bpm, pulse rate 128 ms, QRS 130 ms, QT 400 ms, QTc 400 ms, and P-R-T axes 0, −80, and 105 degrees (Figure 16-2).
Comments
Atrioventricular pacing with biventricular system.
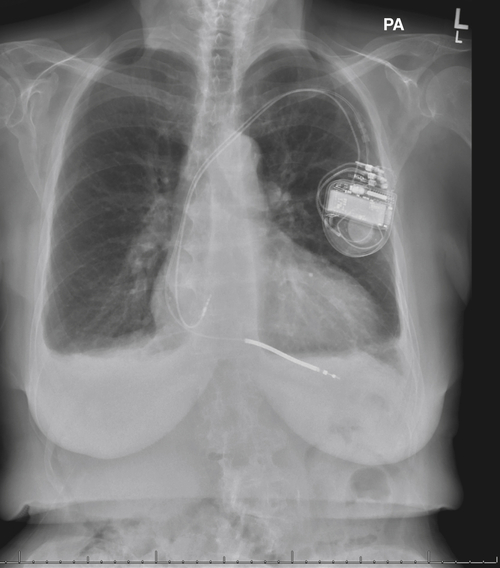
Chest Radiographs Findings
Figure 16-3 shows the heart is mildly enlarged, with left ventricular dominance. Calcification is seen within the aortic knob. An ICD is satisfactorily oriented with right atrial and ventricular leads. The hilar structures are mildly prominent. Small bilateral pleural effusions are seen.
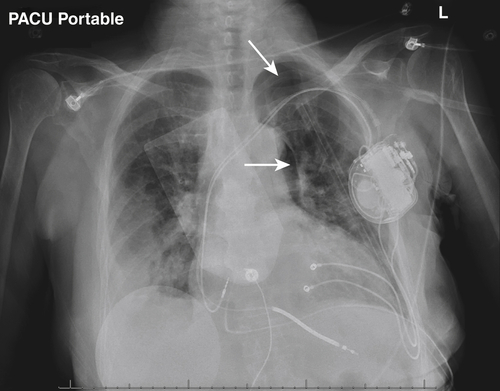
In Figure 16-4, the cardiac silhouette is marginal in size, with intracardiac defibrillator leads directed into the right atrium and both ventricles. Also, a left chest tube had been placed. An abnormal pleural-based opacity is visible in the right lower thorax. Parenchymal consolidation or pleural fluid is not otherwise demonstrated.
Immediately postoperatively there was a patchy right basilar infiltrate and/or a right pleural effusion present with small residual left pneumothorax, see white arrows (see Figure 16-4).
On postoperative day 20 all the previous changes noted on Figure 16-5 have disappeared with no evidence of focal pulmonary consolidation, pleural effusion, or active vascular congestion (Figure 16-6).
Echocardiogram
5 Months Before Surgery



