Transthoracic echocardiogram showing signs of right ventricular strain
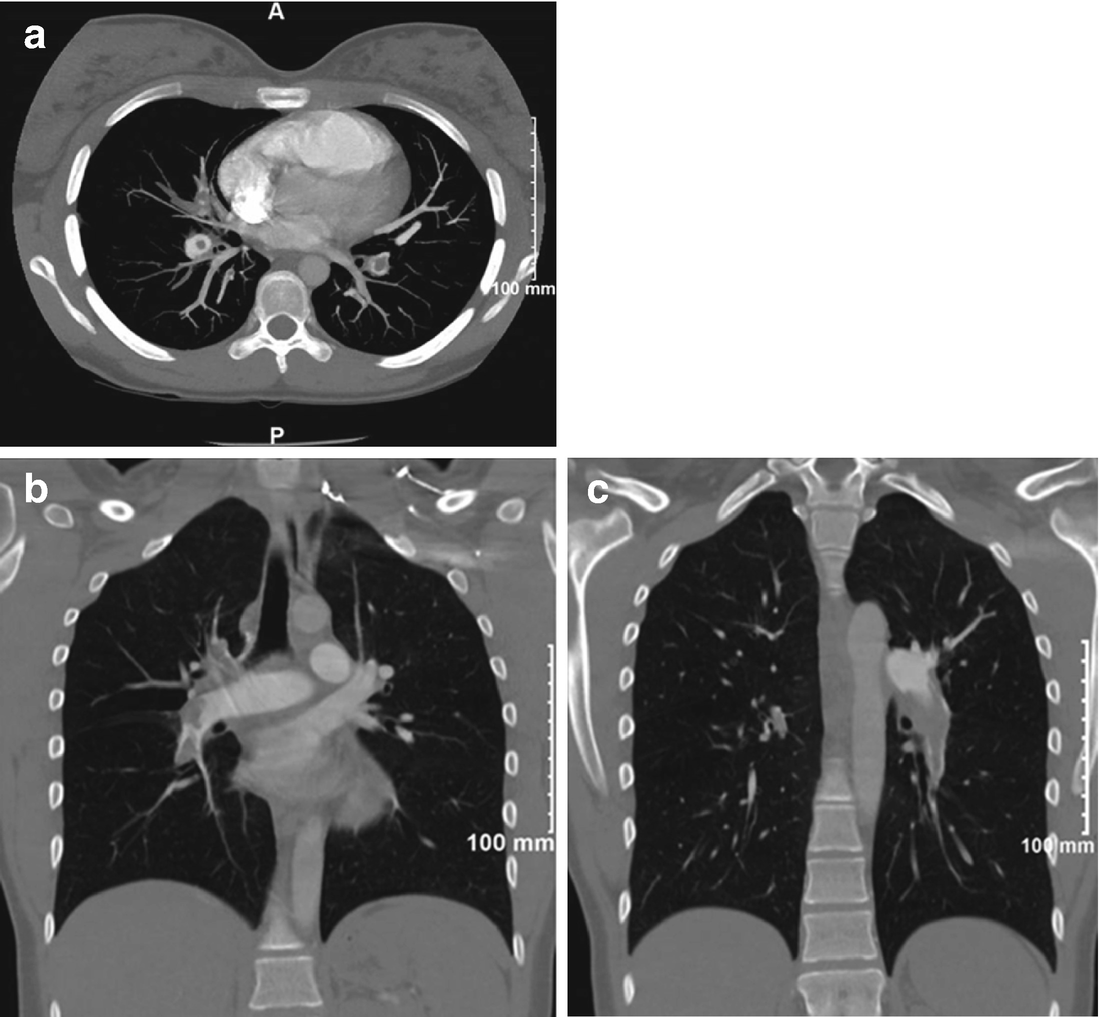
Axial (a) and coronal views (b, c) of the CT angiogram demonstrating extensive proximal vessel intraluminal defects in both lungs consistent with acute pulmonary emboli. There is modest central PA enlargement and RV enlargement, though no significant RV hypertrophy
A duplex venous ultrasound of both lower extremities disclosed the deep veins to be widely patent with normal flow and no evidence of thrombus.
She was admitted to the Intensive Care Unit, after initiating intravenous heparin, with the intention of proceeding with lytic therapy utilizing tissue plasminogen activator (TPA). The clinical history related was consistent with a possible pulmonary embolic event as long as 6 weeks prior; however her presentation was prompted by worsening symptoms that were hemodynamically significant.
She was transferred to a tertiary hospital as the patient and parents requested additional consults prior to moving forward with thrombolysis given lack of consensus in the treatment plan. Hematology and Pulmonary Hypertension/Cardiology consults were obtained and achieved consensus was to withhold lytic therapy for concern that she had acute on chronic pulmonary emboli.
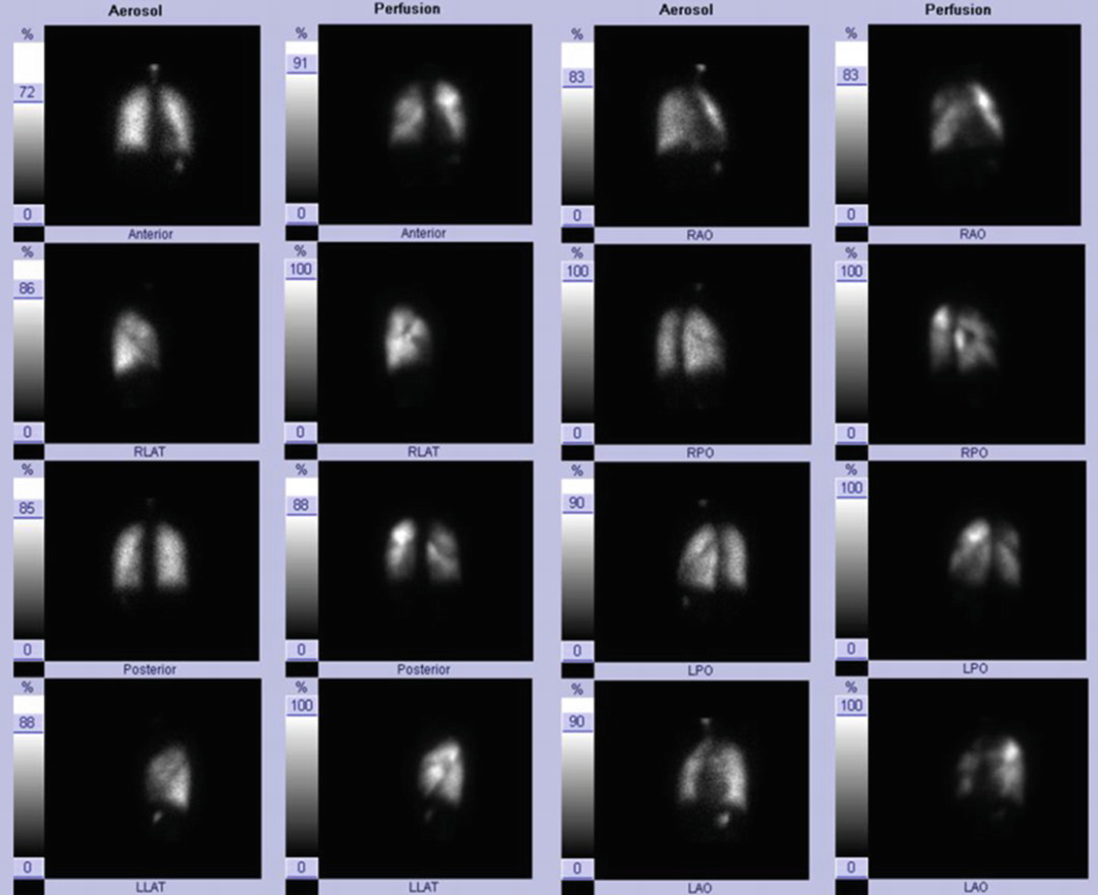
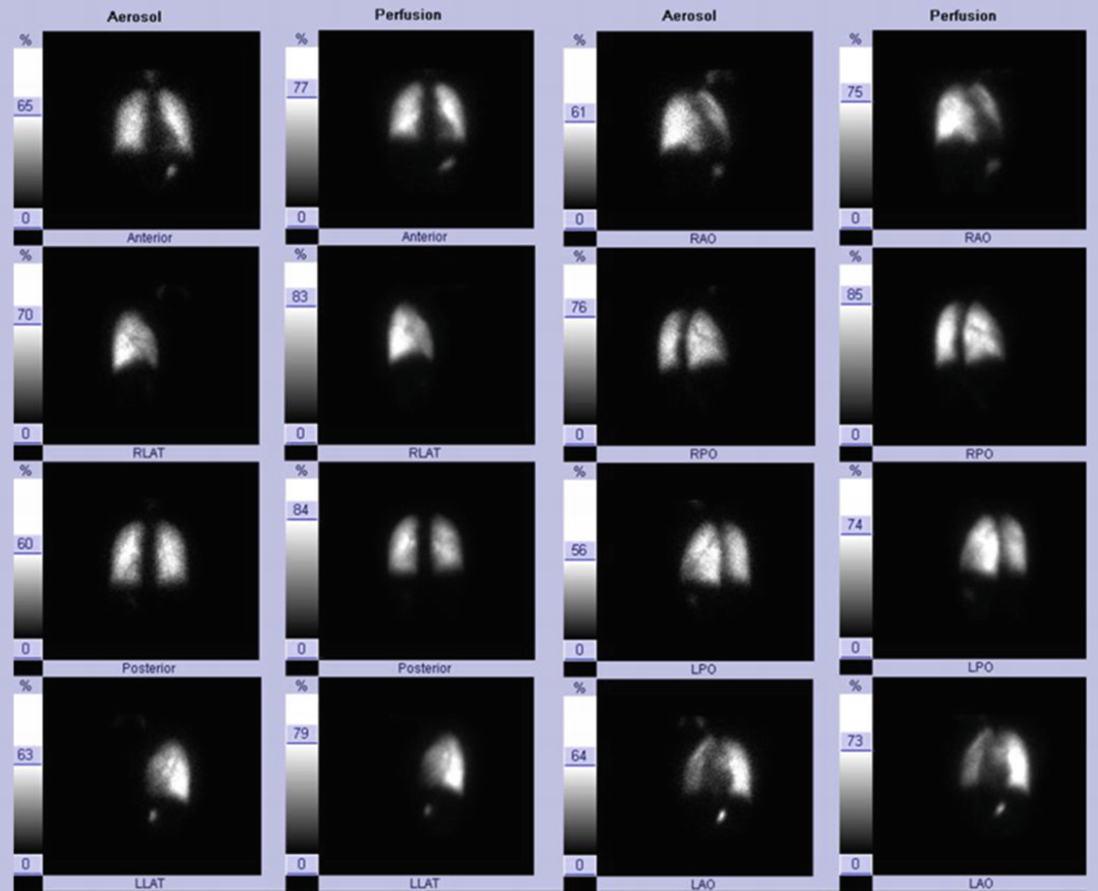
Several unmatched, large perfusion defects, particularly apparent throughout the right lung and medial left lower lobe (posterior view)
On hospital day 6, a right heart catheterization was performed: BP 99/66 mmHg, mean arterial pressure 79 mmHg, HR 77 bpm, pulse oximetry on room air 99%. RA mean 6 mmHg, RV 40/6 mmHg, PA pressure 40/17 (25 mean) mmHg, PCWP 6 mmHg; PA saturation 67.3%; cardiac output 4.5 L/min with a cardiac index 2.43 L/min/m2; transpulmonary gradient was 19 mmHg.
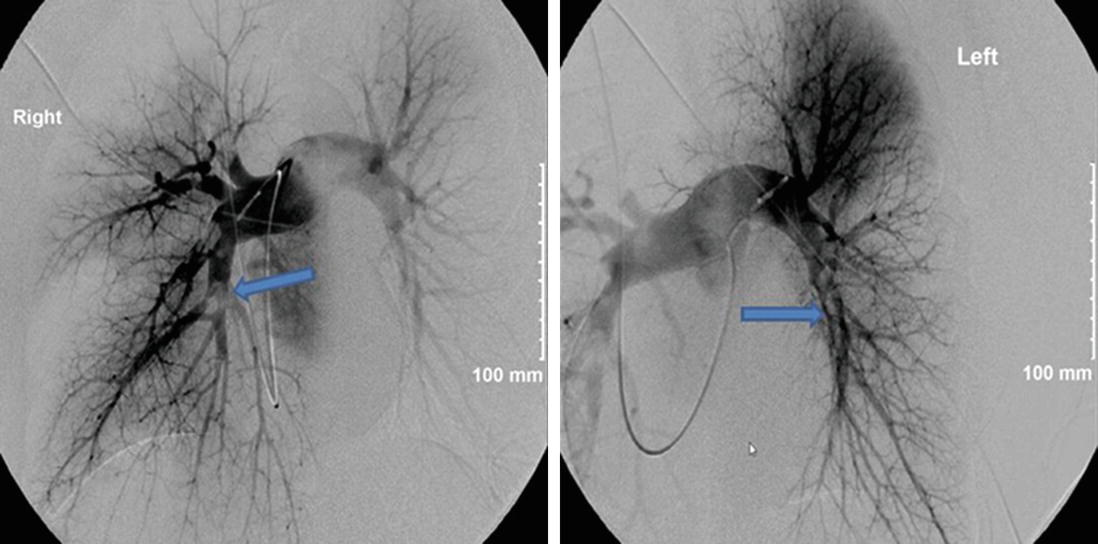
Intraluminal filling defects apparent (arrows) in both descending pulmonary arteries, as well as in the segmental vessels of the right upper lobe, right lower lobe and lingula
By hospital day 12, she was discharged in stable condition. She was at a therapeutic level on warfarin therapy (patient refused Eliquis). She was hemodynamically stable and ambulatory. Thrombolytic therapy was never given, as the consensus of opinions was that she had acute pulmonary emboli on top of significant chronic thrombi. The oral contraceptive (OCP) drugs were discontinued on admission.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


