CASE 15 Transplant Vasculopathy
Case presentation
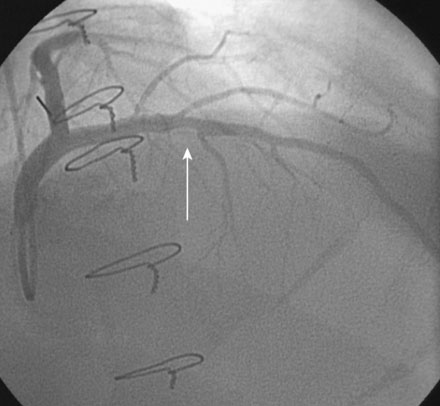
A 61-year-old man underwent orthotopic heart transplantation 16 years ago for ischemic cardiomyopathy. He now presents for his annual routine right and left heart catheterization, coronary angiogram, and endomyocardial biopsy. A coronary angiogram performed 1 year earlier showed only mild atheromatous disease in the left anterior descending artery without significant luminal narrowing (Figure 15-1). He remains free of all cardiac symptoms including chest pain, dyspnea, exercise intolerance, syncope, or edema. Other pertinent medical history includes peripheral vascular disease treated with an aortobifemoral bypass, hypertension, hyperlipidemia, and mild renal insufficiency with a baseline creatinine of 1.4 mg/dL. Medications include simvastatin, diltiazem, azathioprine, cyclosporine, and aspirin. Recent lipid analysis found an LDL of 103 mg/dL and an HDL of 41 mg/dL.
Cardiac catheterization
The right heart pressures were normal. Selective coronary angiography revealed nonobstructive, mild atheromatous disease in the right coronary artery, unchanged from the previous year (Figure 15-2). The left coronary artery showed progression of the lesion in the left anterior descending artery. This lesion now appeared to significantly narrow the lumen (Figure 15-3 and Video 15-1). The circumflex appeared angiographically normal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree