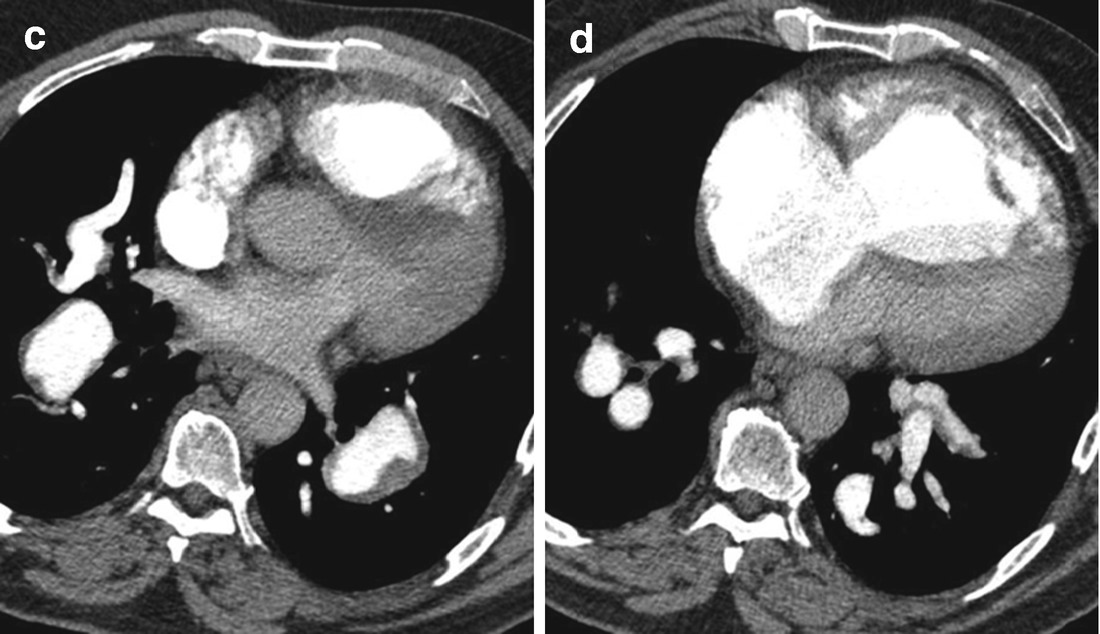
CT angiogram imaging the proximal pulmonary vessels (a), progressing down to the lower lobe arteries (b–d). Lining thrombus is noted throughout the proximal vessels, which does not extend into the enlarged segmental lower lobe arteries. There was no evidence for vessel obstruction or narrowing of the pulmonary vessels with organized clot
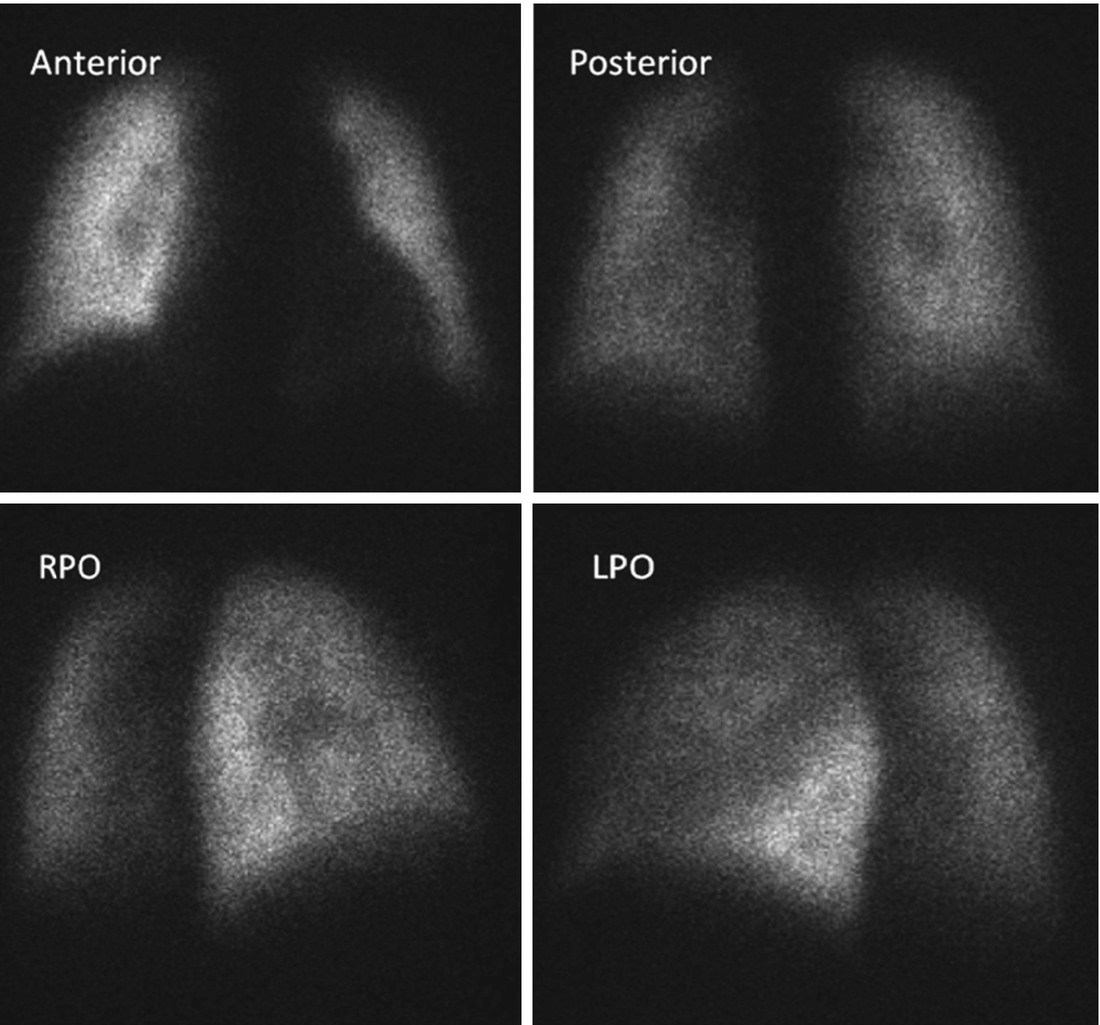
Perfusion scan of the same patient at the same time that the CT angiogram in Fig. 15.1 was obtained. Other than an “imprint” of the enlarged central PAs, the perfusion pattern in both lungs is essentially normal
Lower extremity dopplers were negative and a hypercoagulable workup was positive for a heterozygous Factor V Leiden abnormality.
The patient was ultimately place on diuretics and a soluble guanylate cyclase stimulator in treatment of his pulmonary hypertension. This resulted in an improvement in his overall functional status.
Radiographic Interpretation
CTPA demonstrates features of significant pulmonary hypertension as evidenced by aneurysmal dilation of main pulmonary artery, markedly enlarged right sided cardiac chambers and severe right ventricular hypertrophy. There is reversal of septal curvature with small under-filled left ventricle. There is eccentric non-occlusive clot lining the distal right and left main pulmonary arteries. The segmental pulmonary artery branches are also dilated with thin rim of clot in multiple vessels. No intravascular webs, stenosis or pouch defects were present. Lung windows did not reveal mosaic attenuation. There was no evidence of intracardiac shunt and the pulmonary venous anatomy was normal. Scintigraphy shows mottled perfusion but there are no segmental mismatched perfusion defects that is typical of CTEPH.
The overall appearances are that of PAH with in-situ thrombosis (IST).
Lining clot is a well known complication of long standing PAH (Moser et al.). Proposed mechanism for IST includes wall shear stress from turbulent flow, vascular dilatation leading to stasis and endothelial injury creating a procoagulant environment (Chaouat et al., Archer et al.). Like CTEPH, these clots can also exhibit calcification. Differentiation between the two conditions is crucial as they have entirely different therapeutic options. In CTEPH, the segmental vessels tend to be attenuated whilst PAH is associated with enlarged proximal vessels and peripheral pruning. Other angiographic features of CTEPH such as truncation of segmental arteries, variation in size of segmental vessels, webs, stenosis and pouch defects are absent in PAH. Congenital heart disease can also be associated with IST and is seen in about one-fifth of the patients with Eisenmenger’s syndrome . Hence, it is important to make a thorough search for the presence of intracardiac shunts.
Clinical Comments
Though CTEPH has been defined as pulmonary hypertension in the presence of radiographic evidence for chronic thromboembolic disease , the case presented here is an example of how that definition can sometimes be misconstrued. What is present in this patient is organized thrombus lining enlarged central pulmonary vessels—in-situ and non-embolic. It is a consequence of longstanding pulmonary hypertension and not the cause of it. Most often this is seen in congenital heart disease with Eisenmenger’s physiology that has resulted in massively enlarged proximal pulmonary arteries (see Case 19, Chap. 19). How this develops is not completely understood. As pointed out by Dr. Gopalan, it is possible that the blood flow juxtaposed to the enlarged vessel is “stagnant” enough to allow thrombosis to occur; or possibly there’s an endothelial injury of the proximal vasculature which promotes clot formation. Either consideration is speculative.
Though the extent of thrombus visualized by CT can be impressive, as the vessels are examined distally, most often the lining thrombus disappears leaving the vessels intact and unobstructed. As blood flow through these vessels is unimpeded, the relatively normal perfusion pattern seen on lung scintigraphy is not surprising. Consequently, logic dictates and previous experience has demonstrated that surgical endarterectomy of this lining thrombus provides no pulmonary hemodynamic benefit and should be considered contraindicated.
Point of Emphasis
Lining thrombus within enlarged central pulmonary vessels is typically unobstructive and is not the basis for a patient’s pulmonary hypertension, but a consequence of it.
Diagnosis
- 1.
Lining thrombus within enlarged central pulmonary arteries.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


