Body mass index
Skin condition
Presence of studs and other jewellery that cannot be removed
Nutritional status
Allergies
Pre-existing medical conditions
Physical or other mobility issues
Pre-existing prosthesis or implanted devices such as pacemakers
Pre-existing external factors such as urinary catheters, drains from previous surgery
From Association of Perioperative Room Nurses (2008).
The length of time that it is anticipated that the patient will be in the surgical position
The surgical position that is required
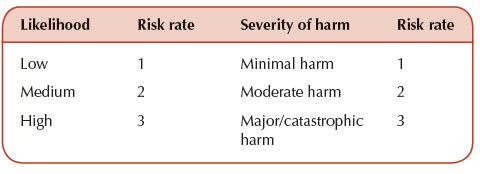
Table 13.2 Simple matrix for a risk scoring system.
It is important that perioperative practitioners are involved in undertaking the risk assessments as they are the people most likely to be familiar with the equipment and processes that are being assessed. It is often the case that the risk assessment process is thought to be complicated, but it actually comprises five distinct and separate steps as follows:
Planning the assessment enables a practitioner to clearly identify the activity or task under scrutiny, which in turn can assist the practitioner in identifying the hazards associated with the activity or task. It is important to note the significance of each hazard, as well as evaluating the risk associated with the hazard. A recognised risk scoring system such as high, medium or low will facilitate a prediction of the likelihood of harm and the severity of harm that will occur, thus creating a risk score (Champion 2000, Health and Safety Executive 1997). This can be measured in a simple matrix as shown in Table 13.2.
The level of risk can be assessed by a simple multiplication of the risk rates of the likelihood of harm and the severity of harm, which can then allow a warning system of red, amber and green to be used to assess the risk level as high, medium or low. For example, a risk score of 6–9 would be classed as red and require immediate action to reduce the risk, an amber risk would range between 3 and 6 and require action within an agreed timescale whereas a score of 1–3 would be identified as green and monitored to ensure that it remains at this level.
Having established the risk assessment and management principles to be applied to patient positioning, it is now pertinent to consider the range of patient positions available. The purpose of a specific surgical position is to ensure that the maximum view of the operative field is obtained whilst maintaining the comfort and safety of the patient at all times (Adeeji et al. 2010). A further compromise in the choice of patient position can be related to the type of anaesthetic used and the access that the anaesthetist will require during the procedure. The range of key surgical positions is described in the following section.
Key Surgical Positions
The key surgical positions are lateral, lithotomy, prone, supine, Trendelenburg and reverse Trendelenburg, with supine being the most commonly used position for perioperative procedures (Smith 2005).
Lateral
In this position, the patient is placed on their side and is supported by the use of a table accessory positioned against the patient’s abdomen, with a further support against their lower back. The upper arm is supported in a gutter support. Care must be taken to ensure that the lower limbs are protected from undue pressure by placing a suitable pillow or other pressure-relieving device between the legs to reduce pressure on bony prominences, as well as the use of gel pads to protect against pressure on the lower heel (Smith 2005). This position is often used in thoracic surgery, some renal surgery and also in hip surgery.
Lithotomy
In this position the patient is initially placed in a supine position and then the legs are raised and the feet supported in stirrups or other leg supports, thus allowing the lower end of the table to be removed in order to facilitate access for gynaecological, urological and some lower bowel surgical procedures. It is important that the patient’s legs are moved simultaneously into position on the leg supports, which are at the same height, in order to reduce the risk of flexion beyond 90°. If the patient is to be positioned in lithotomy poles, then their legs should be positioned on the outside of the poles in order to prevent pressure on the peroneal nerve. The patient’s buttocks must be aligned with the break in the table, and in a position that will support the sacrum, once the base of the table has been removed. The patient’s arms should be supported on arm boards with less than a 90° angle in order to prevent injury (AfPP 2007, Association of Perioperative Room Nurses 2008).
Prone
The prone position is used for some neurosurgical, spinal and vascular procedures. The patient will initially be in the supine position, prior to being rolled into a face down position. It is essential that sufficient people are present in order to position the patient safely, including ensuring that the patient’s cervical alignment is maintained and that the patient is positioned on a headrest which allows access to the airway. It should be noted that one person should be in command of the instructions to move the patient, and that this person is most likely to be the anaesthetist, as he or she has responsibility for the patient’s airway. The headrest should provide adequate protection to the forehead, eyes and chin. The patient’s arms should be positioned by their sides or, if this is not possible, then on arm boards, with an abduction of less than 90°, and with the elbows flexed and palms facing downwards. Placing the patient’s arms above their head can cause injury to the brachial plexus (AfPP 2007, Association of Perioperative Room Nurses 2008). One person, preferably the anaesthetist, is in control of the moving and turning of patients.
Supine
In this position, the patient lies flat and it is important that their spine is kept in alignment, and that the patient’s head and upper body are in alignment with their hips and that their legs are parallel. Heel supports should be provided to reduce pressure and the arms should be placed on suitably aligned arm boards. Pregnant women may require a 20° tilt to the left in order to prevent pressure on the inferior vena cava (AfPP 2007, Association of Perioperative Room Nurses 2008, Pirie 2010).
Trendelenburg
The Trendelenburg position is often used for pelvic surgery where the patient is positioned in a supine position initially and then the operating table is tilted to a head down position which does not exceed a 20° tilt. It is essential that a non-slip mattress is used in order to prevent the patient from moving either during positioning or during the procedure itself (AfPP 2007, Pirie 2010).
Reverse Trendelenburg
This position, as the name suggests, is where the patient is positioned in the supine position prior to being tilted into a head up position. This position is used for head and neck surgery such as thyroid surgery as well as for some shoulder and abdominal surgery, such as cholecystectomy (AfPP 2007, Pirie 2010).
It is important to note that there are some variations to the above positions which are also recognised perioperative positions. These are described below.
Dorsal recumbent position
This is similar to the supine position, but at least one arm will be positioned at the side of the patient, with the other arm extended on an arm board to facilitate venous access. The arm that is placed at the side of the body should not be subjected to undue pressure. The elbows should also be protected to prevent injury. This position can be used in abdominal surgery (AfPP 2007).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


