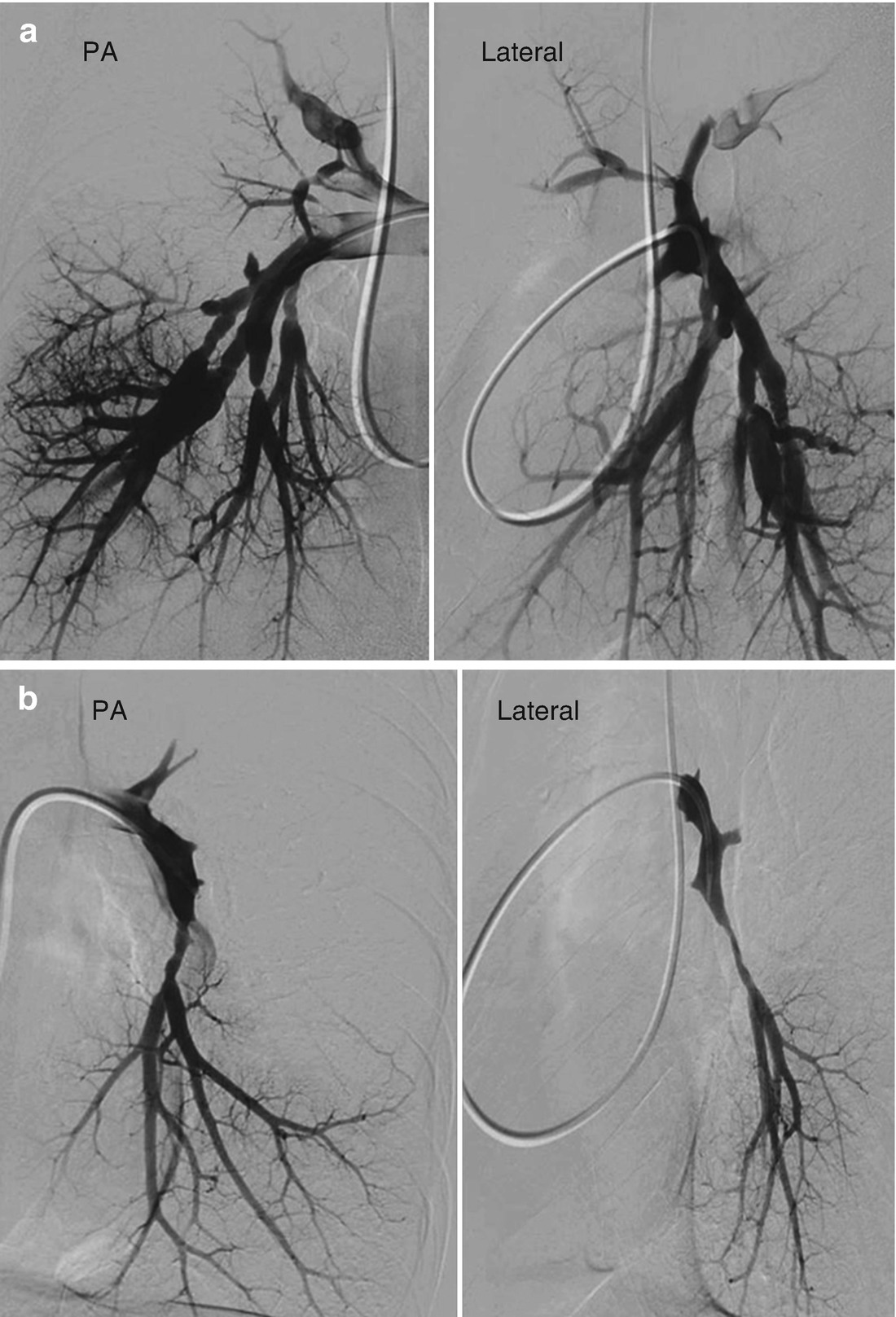
Lung scintigraphy demonstrating a number of unmatched perfusion defects, predominantly involving the upper lobes, lingula and right middle lobe
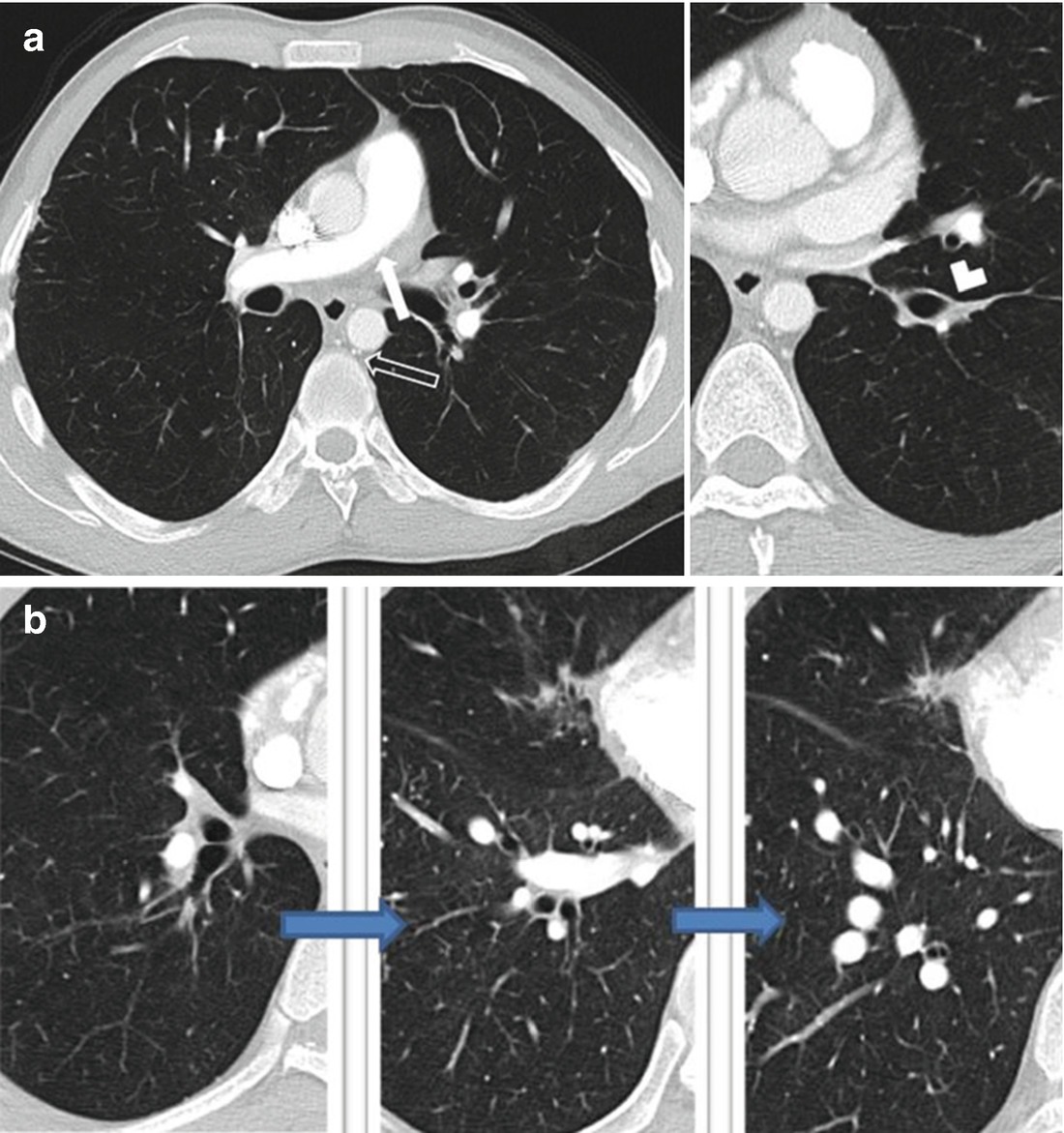
(a) Right main pulmonary artery narrowing (white arrow) throughout its course with marked vessel narrowing of the left descending PA (chevron). Bronchial arterial collateral vessels also noted. (open arrow). (b) Proximal to distal (left to right) axial images of the CT angiogram shown in (a). Small right descending PA to attenuated proximal RLL segmental vessels to dilatation of the more distal segmental vessels of the right lower lobe. No CT evidence for chronic thrombus
On initial evaluation at a CTEPH center he reported some improvement in exercise tolerance, but remained WHO functional class III with one block DOE and exertional lightheadedness. Additional PMH included left spontaneous pneumothorax treated with VATS (report of evaluation for Marfan’s negative at that time), chronic hoarseness, mild thrombocytopenia, questionable Protein S deficiency in the setting of warfarin therapy, and abnormal LFTs with a liver ultrasound demonstrating early cirrhotic changes. His family history was remarkable for a sister who required surgery as a child for a “hole in her heart”. He previously drank 6–12 beers daily, but had decreased his alcohol intake substantially and continued to smoke marijuana.
Physical exam revealed a very tall and thin Hispanic male comfortable at rest. HR 65, BP 136/67, RR 16, SpO2 96% on room air. There was no JVD, but a carotid bruit vs. a transmitted murmur over his left carotid artery was auscultated. Lung fields were clear with loud pulmonary flow murmurs noted anteriorly and posteriorly in both lungs. There was no RV lift, S1 was normal with a loud second heart sound and a soft systolic murmur without gallop. Abdominal exam was normal without evidence of bruits. Extremities revealed no edema, no bruits over proximal arteries, and pulses were all strong and symmetric except for a diminished right dorsalis pedis and posterior tibialis pulses.
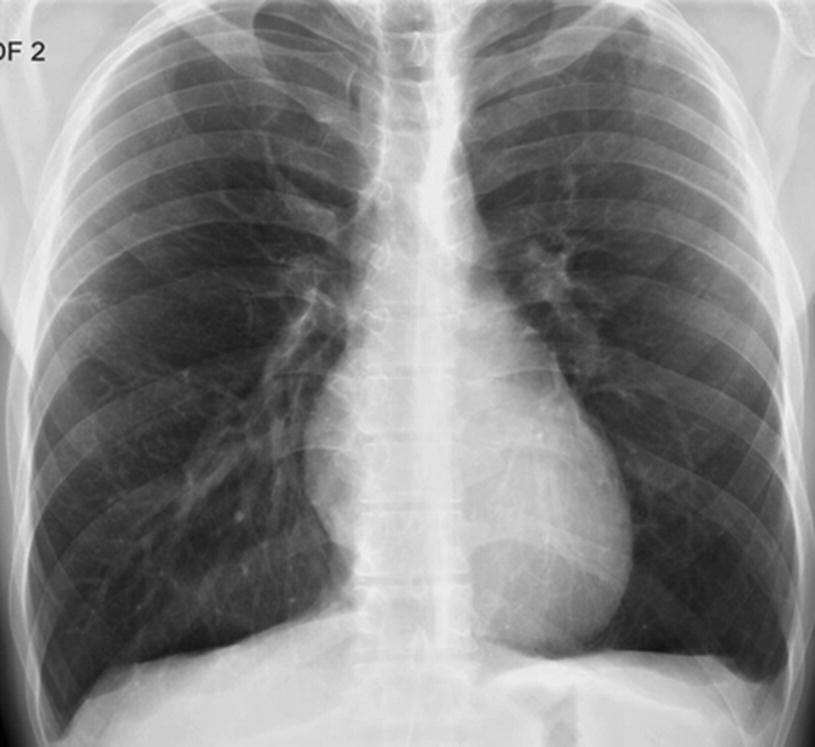
PA chest radiograph: no central pulmonary artery enlargement despite the severe pulmonary hypertension documented by right heart catheterization
An echocardiogram showed normal right and left sided chamber size and function, normal valvular function and estimated RV systolic pressure of 121 mmHg. Repeat right heart catheterization was performed: RA 5, RV 110/6, PA 110/16 (mean 43), PAOP 7, cardiac output 4.25 L/min, cardiac index 2.19 L/min/m2, PVR 678 dynes s cm−5, PA saturation 70%.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


