1
Dyspnea
OBJECTIVES
 Define dyspnea and its pathophysiologic relationship to various disease processes.
Define dyspnea and its pathophysiologic relationship to various disease processes.
 Identify types of respiratory disease by the recognition of spirometric patterns.
Identify types of respiratory disease by the recognition of spirometric patterns.
 Identify appropriate tests used in the systematic evaluation of dyspnea.
Identify appropriate tests used in the systematic evaluation of dyspnea.
GENERAL CONSIDERATIONS
Dyspnea is a sensation of breathlessness or subjective “shortness of breath.” It defies strict definition with many individual descriptions and varies widely among patients for comparable objective dysfunction. The American Thoracic Society (ATS) has defined dyspnea as “a term used to characterize a subjective experience of breathing discomfort that is comprised of quantitatively distinct sensations that vary in intensity.” The sensation of breathlessness can be experienced by healthy subjects with exercise or at high altitudes and those with diseases that affect the respiratory, cardiac, endocrine, renal, neurologic, hematologic, or rheumatologic systems. It is a frequent clinical complaint. Occasionally, a source cannot be clearly identified, and dyspnea is attributed to psychophysiologic disturbances.
ETIOLOGY & PATHOGENESIS
Dyspnea in patients with chronic obstructive pulmonary disease (COPD) is due to narrowing of the airways, increased airway resistance, and reduction of lung elastic recoil. Very often, concominant hyperinflation is seen, which alters respiratory muscle mechanics, thereby increasing the sensation of dyspnea. Infiltration of the lung parenchyma in diffuse lung disease such as pulmonary fibrosis can also result in similar ventilatory impediment due to increased elastic work of breathing. This is also seen in conditions causing acute respiratory distress syndrome (ARDS) and pulmonary edema with congestive heart failure (Table 1–1). Excessive secretions and inability to clear such secretions can compromise airways and increase airway resistance. Chest wall mechanics can also be compromised by pleural disease and cause dyspnea. Some patients with chronic lung disease have increased minute ventilation at rest and on exertion due to increased dead space (wasted ventilation), increased carbon dioxide production, and enhanced drive to breathe.
The sensation of dyspnea increases when the demand to breathe is disproportionate to the requirement. Increased work of breathing resulting from an imbalance between afferent inputs and respiratory muscle output due to poor nutrition and muscle strength can contribute to the sensation of dyspnea. Common to the processes causing metabolic acidosis, such as aspirin, methanol ingestion, increased lactic acidosis due to poor tissue perfusion, overproduction of ketones secondary to metabolism of fatty acids (eg, diabetic ketoacidosis, alcoholism, or starvation), renal failure (decreased excretion of hydrogen ions), or bicarbonate loss (eg, diarrhea, renal dysfunction, or pancreatic disease), is an increase in hydrogen ions, which stimulate arterial receptors, especially those in the carotid bodies. This respiratory compensation is often appreciated or perceived as dyspnea.
PATHOPHYSIOLOGY & MECHANISM OF DYSPNEA
 Breathing is an unconscious act; we are only aware of our breathing effort when something is wrong. Many respiratory conditions can present acutely with the sensation of dyspnea. Dyspnea is not a single sensation and the mechanism of dyspnea is not well understood. Similar to pain, dyspnea appears to be multidimensional encompassing unpleasantness and emotional impact. Dyspnea has two dimensions, sensory and affective, and both can be independently identified in the laboratory and in clinical situations. Also, it is a perception or subjective experience and it must be explained by human experiments. New brain imaging studies indicate that the sensation of different respiratory efforts is perceived in several areas of the brain stem and sensory cortex with dyspnea resulting when the degree of stimulation in respiratory-related neurons is perceived as being excessive. Stimulation may arise from different situations (eg, exercise, hypoxia, or breath-holding), medical conditions (eg, increased airway resistance, decreased compliance, or increased work of breathing), physical discomfort (pain), metabolic changes (acidosis), emotional discomfort, excitement, and depression. Receptors in the heart may also give rise to perceptions of dyspnea (orthopnea) since awareness of breathing may occur with apparently normal lungs and gas exchange.
Breathing is an unconscious act; we are only aware of our breathing effort when something is wrong. Many respiratory conditions can present acutely with the sensation of dyspnea. Dyspnea is not a single sensation and the mechanism of dyspnea is not well understood. Similar to pain, dyspnea appears to be multidimensional encompassing unpleasantness and emotional impact. Dyspnea has two dimensions, sensory and affective, and both can be independently identified in the laboratory and in clinical situations. Also, it is a perception or subjective experience and it must be explained by human experiments. New brain imaging studies indicate that the sensation of different respiratory efforts is perceived in several areas of the brain stem and sensory cortex with dyspnea resulting when the degree of stimulation in respiratory-related neurons is perceived as being excessive. Stimulation may arise from different situations (eg, exercise, hypoxia, or breath-holding), medical conditions (eg, increased airway resistance, decreased compliance, or increased work of breathing), physical discomfort (pain), metabolic changes (acidosis), emotional discomfort, excitement, and depression. Receptors in the heart may also give rise to perceptions of dyspnea (orthopnea) since awareness of breathing may occur with apparently normal lungs and gas exchange.
Table 1–1. Pathophysiologic correlates of disease causing dyspnea
Structural or mechanical interference with ventilation |
Obstruction of flow |
Emphysema |
Asthma |
Chronic bronchitis |
Tracheal (after prolonged mechanical ventilation, vocal cord dysfunction) |
Endobronchial disease, primary lung carcinoma, foreign body |
Restriction to lung or chest wall expansion |
Intrinsic: diseases involving lung parenchyma |
Interstitial fibrosis |
Acute respiratory distress syndrome |
Congestive heart failure |
Extrinsic: processes not involving lung parenchyma |
Kyphoscoliosis |
Obesity |
Ascites |
Pregnancy |
Pleural fibrosis |
Increases in dead space ventilation |
Emphysema: obstruction of airflow |
Pulmonary embolus: interruption of blood flow |
Respiratory muscle weakness |
Poliomyelitis |
Neuromuscular disease |
Systemic diseases |
Guillain-Barré syndrome |
Increases in respiratory drive |
Hypoxemia: secondary to any cause |
Exercise |
Metabolic acidosis: diabetic ketoacidosis and renal failure |
Significant decreases in hemoglobin or cardiac output |
Psychological disturbances |
Anxiety/panic attacks |
Depression and somatization disorders |
Source: Adapted with permission from Stulbarg MS, Adams L. Dyspnea. In: Murray JF, Nadel JA, eds. Textbook of Respiratory Medicine. Vol. 1, 3rd ed. Philadelphia, PA: WB Saunders; 2000:511–528.
The increased afferent stimulation of the respiratory complex from a variety of receptors (chemoreceptors, proprioreceptors, or emotions) results in increasing efferent neural drive to the respiratory muscles. Additional stimuli of other afferent pathways can contribute (eg, bronchospasm, inflammation, pulmonary hypertension, or lung edema). This information is simultaneously relayed to sensory areas within the cortex.
The sense of respiratory effort intensifies with increases in central efferent respiratory motor activity. This sense of effort is proportional to the ratio of the pressures generated by the respiratory muscles to the maximum pressure-generating capacity of these muscles. Mechanical support during exercise therefore reduces the sensation of dyspnea. Externally supported increases in minute ventilation (by a mechanical device) are associated with little or no dyspnea.
The final perception of dyspnea may best relate to total neural traffic. Both the “sense of effort” (augmented requirements to overcome mechanical constraints or muscle weakness) and the “urge to breathe” (hypoxia, hypercapnia, airway compression, and anxiety) contribute to the global perception of dyspnea. There is polymorphism in neurotraffic with some (patients) producing greater neurotraffic for similar experience. This may explain individual “panic attacks” in certain patients. The addition of oral or parenteral opioids reduces dyspnea in patients with severe disease whereas the use of antidepressants may reduce dyspnea in some patients.
Dyspnea is worse when unexpected or perceived to be dangerous. Adaptation or acclimatization seems to occur with hypoxemia, exercise conditioning, and some mechanical constraints.
Thus, dyspnea increases when ventilatory impedance increases as during an acute asthma attack, when ventilatory demand increases as during exercise, when respiratory muscle function is abnormal as in hyperinflation states, and when perception of dyspnea is increased as during an anxiety attack. The correlation between dyspnea and objective measures of lung and cardiac function is weak.
DIAGNOSTIC & CLINICAL CONSIDERATIONS
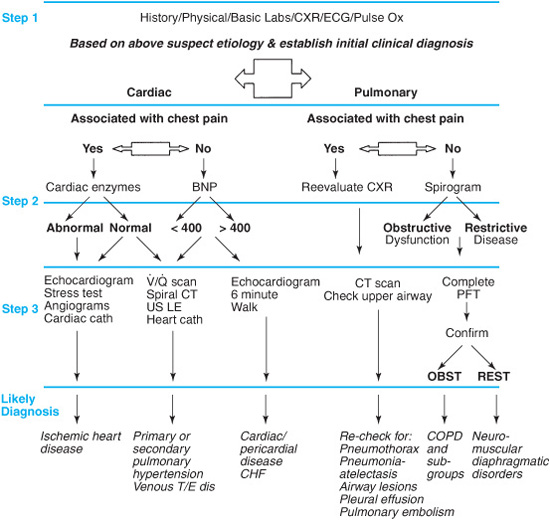
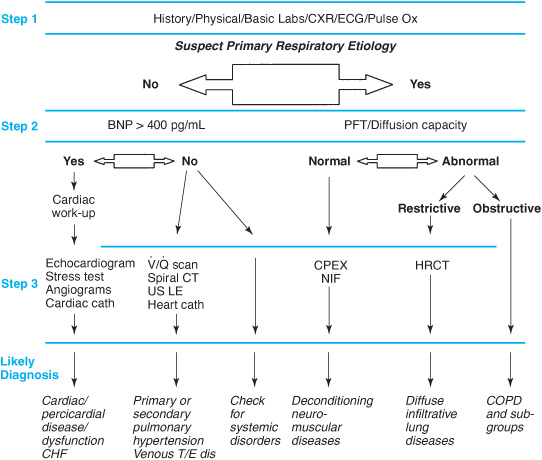
An understanding of basic respiratory physiology enables the clinician to categorize and evaluate dyspnea. Basic concepts such as increased respiratory drive, respiratory muscle weakness, dead space ventilation, and mechanical impairment of ventilation, all contribute to an understanding of the underlying causes and mechanisms of dyspnea. It is possible to narrow the differential diagnosis and evaluation of dyspnea by asking whether the symptoms are acute or chronic (see Figures 1–1 and 1–2). Acute changes are more likely to be seen in congestive heart failure, myocardial infarction, exacerbations of COPD, asthma attacks, pulmonary embolism, and pneumonia. Dyspnea is usually recognized as chronic when it is present for at least 4–8 weeks. Common causes and observed frequencies for chronic dyspnea are listed in Table 1–2.
Evaluation of the History
A comprehensive history is required and will help to define the timing, precipitating or aggravating factors, related conditions, severity of symptoms, their relationship to activity, and any identifiable alleviating factors. Patients with certain diseases tend to describe the shortness of breath in similar terms (Table 1–3), but the reliability of specific descriptions is suspect. Nocturnal dyspnea may be related to several disease processes, such as asthma, congestive heart failure, gastroesophageal reflux, or nasal congestion. In the supine position, dyspnea may be related to something that upwardly displaces the abdominal contents, such as pregnancy, ascites, diaphragmatic paralysis, or redistribution of intravascular volume to the central circulation that is not compensated due to a failing heart. If symptoms are intermittent, the clinician should consider reversible diseases such as asthma (bronchoconstriction), heart failure, or recurrent pulmonary emboli. Progressive symptoms usually signal more chronic diseases, such as interstitial pulmonary fibrosis, sarcoidosis, COPD, amylotrophic lateral sclerosis, or cancer.
Figure 1–1. Algorithm for evaluation of acute dyspnea. See list of abbreviations at the end of the book.
Dyspnea that has its onset in conjunction with physical activity is generally of physiologic origin. For example, dyspnea may be due to deconditioning, anemia (decreased oxygen delivery), or exercise-induced asthma. If the patient complains of shortness of breath that is independent of physical activity, the clinician should consider psychological problems. If the dyspnea is clearly out of proportion to objective findings, it may be related to personal gain or litigation (malingering).
Figure 1–2. Algorithm for evaluation of a patient reporting chronic dyspnea. See list of abbreviations at the end of the book.
Asthma | 20–30 |
Cardiac | 15 |
COPD | 5–15 |
Interstitial lung disease | 5–15 |
Deconditioning and obesity | 5–15 |
Psychophysiologic | 5–25 |
Unexplained upper airway | 5–7 |
Pulmonary vascular | 5 |
Neuromuscular | 5 |
Endocrine (hyperthyroid) and GI | 5 |
Note: COPD, chronic obstructive pulmonary disease; GI, gastrointestinal.
Table 1–3. Often-used patient descriptions of dyspnea as reported in asthma
My breathing is heavy |
I feel a hunger for more air |
I feel out of breath |
I have an uncomfortable awareness of my breathing |
I am gasping for breath |
My chest feels tight |
I can’t take a deep breath |
My breathing is rapid |
I can’t get enough air |
I feel I am smothering or suffocating |
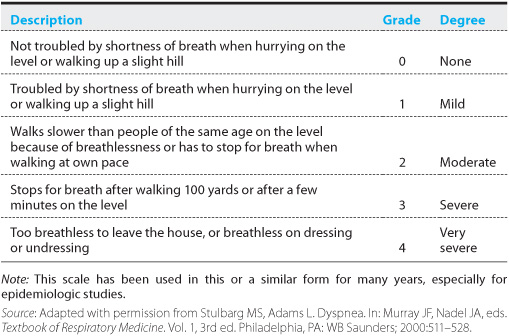
Table 1–4. American Thoracic Society shortness of breath scale
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree