Chapter 72 Chest Tube Insertion and Management
Indications and Contraindications
Conditions associated with acute or severe respiratory compromise are considered absolute indications for chest tube placement and include tension pneumothorax, large symptomatic pneumothorax, hemothorax, empyema, and previous surgical violation of the pleural space (Box 72-1). In addition, under less clear-cut circumstances, appropriate judgment and experience will be required to help determine whether a chest tube is needed or not. Alternatives to chest tube placement, such as observation, thoracentesis, or formal operative drainage, must be considered and the choice individualized according to the clinical situation. Special caution is necessary when the patient’s preoperative assessment findings point to an increased possibility of coagulopathy, intrapleural adhesions, or abnormal intrathoracic anatomy. The only contraindications to chest tube placement are a fused pleural space and lack of operative personnel with adequate experience in use of the technique for a safe and effective procedure. In considering placement of a chest tube, either of these circumstances should prompt consultation with a thoracic surgeon.
Technique
Selection of Drain Tube
At present, the most common tube used for chest drainage is a Silastic tube with multiple side holes. It usually has a linear radiopaque stripe running through the most proximal hole (allowing its location to be identified on chest radiographs) and markings to indicate distance in centimeters from the most proximal hole (Figure 72-1). These tubes range in size (gauge) up to 40 French (40F). Of note, some tube insertion kits come with a central trochar within the chest tube. Routine use of this trochar is unnecessary, can be dangerous, and is to be discouraged. Smaller chest tubes (14F or smaller) also are available, which can be placed using a Seldinger technique without the need for blunt dissection.

Figure 72-1 Silastic chest tubes. Top to bottom: Multiholed straight and angled Silastic chest tubes and Kelly clamp.
Drain Insertion Site and Patient Positioning
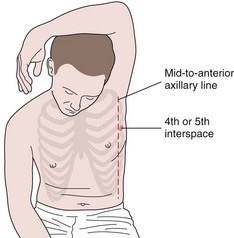
Generally, the optimal site for placement of a chest tube is through the fourth or fifth interspace in the anterior to midaxillary line just beyond the lateral edge of the pectoralis muscle and breast tissue (Figure 72-2). This insertion site has the advantage of relatively easy access and avoids the discomfort of a more posteriorly placed tube in patients who often are primarily lying supine in a hospital bed. In addition, it usually is high enough to avoid inadvertent subdiaphragmatic placement yet low enough to adequately drain fluid. Of note, in patients who are primarily lying supine in bed with free-flowing pleural fluid collections, the interspace level of placement of the chest drain is much less important than ensuring the posterior positioning of the tube within the pleural space. Placement of a chest tube in the second or third interspace anteriorly is to be avoided if possible. Such placement does not provide any advantage over the lateral position described previously and is significantly more painful and disfiguring for the patient.
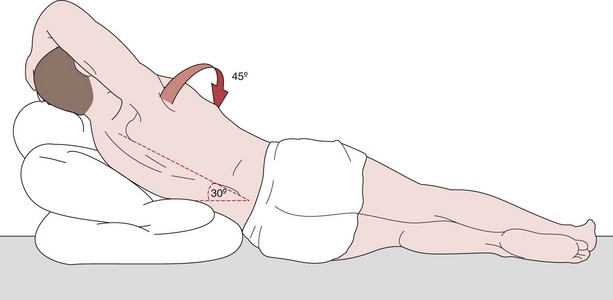
For elective chest drain insertion, the patient should be kept in a relatively comfortable position that facilitates placement of the tube in the location described earlier. Usually, this can be achieved by placing the patient supine or in a semi-Fowler position (with thorax and head elevated 30 to 45 degrees) with the involved side elevated approximately 30 to 45 degrees on wedges or pillows. To improve access to the lateral chest wall, the patient’s arm on the involved side is brought above the head (Figure 72-3). As with most thoracic procedures, the operator should stand at the patient’s back.
Preparation, Anesthesia, and Incision
Before positioning of the patient, all necessary equipment should be made available (Box 72-2). A deliberate pause should be taken to verify the patient’s identity and to confirm the procedure and correct operative side. When possible, the most recent chest radiograph should be posted in a readily visible location as a separate safety measure to avoid wrong-sided procedures.
Box 72-2
Instrument Requirements for Chest Tube Insertion
Drain Insertion
Once the parietal pleura have been breached, the clamp is withdrawn in the open position. The next step is to insert the operator’s index finger into the pleural cavity to ensure pleural entry (to exclude subdiaphragmatic placement) and assess for the presence of pleural adhesions and pleural lesions or nodularity (Figure 72-4). The chest tube can then be guided into place by use of the Kelly clamp, as illustrated in Figure 72-5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree