Bilateral Hilar Mass
Christopher M. Walker, MD
DIFFERENTIAL DIAGNOSIS
Common
Sarcoidosis
Pulmonary Arterial Enlargement
Less Common
Lymphadenopathy Associated with Infections
Lymphoma
Rare but Important
Silicosis/Coal Worker’s Pneumoconiosis
Berylliosis
Lymphadenopathy Secondary to Metastatic Disease
Angioimmunoblastic Lymphadenopathy
Amyloidosis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Bilateral hilar mass usually secondary to pulmonary artery or hilar lymph node enlargement
Lobulated contour in lymph node enlargement
Smooth contour in pulmonary arterial enlargement
Helpful Clues for Common Diagnoses
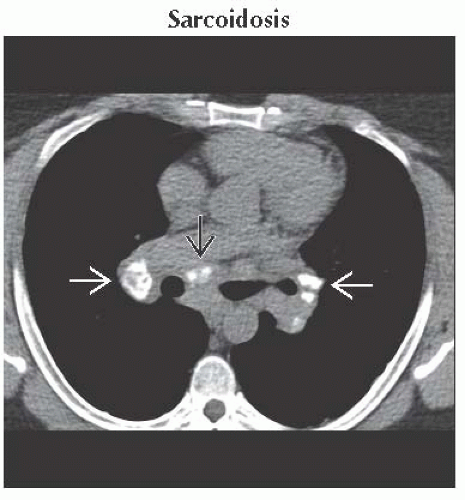
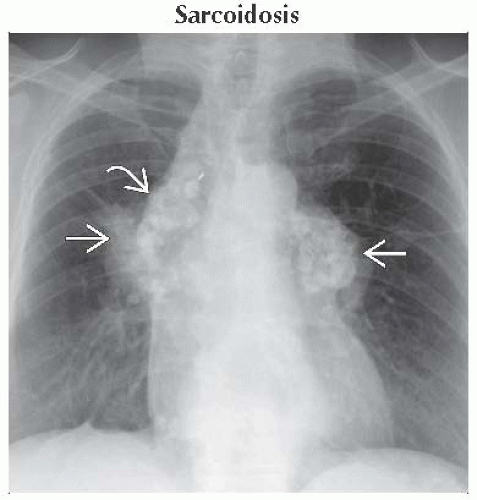
Sarcoidosis
Systemic disease of unknown etiology
Common in African-American females of childbearing age
Most patients present with thoracic lymph node enlargement
50% have associated lung disease
Hilar lymph node enlargement in ≥ 80%
Lobulated and symmetric
± calcification
1, 2, 3 sign (Garland triad)
Right paratracheal (1), right hilar (2), and left hilar (3) nodal enlargement
CT findings
Symmetric hilar and mediastinal nodal disease
25-50% of nodes show calcification
Eggshell calcification
Lung nodules (noncaseating granulomas) along fissures, subpleural lung, and bronchovascular bundles
Upper lung predominant
Pulmonary Arterial Enlargement
CT angiogram diagnostic
Etiologies include
Pulmonary arterial hypertension, primary and secondary causes
Left-to-right shunts
Idiopathic with no associated pulmonary hypertension
Most common cause is pulmonary arterial hypertension
Radiographic and CT findings
Dilatation of central pulmonary arteries with pruning and tapering of distal vessels
Main pulmonary artery ≥ 29 mm
Main pulmonary artery ≥ size of ascending aorta
Calcification of pulmonary arterial wall seen with irreversible longstanding disease
± mosaic perfusion due to associated small vessel disease
Examples of left-to-right shunts
Atrial septal defect
Ventricular septal defect
Partial anomalous pulmonary venous return
Patent ductus arteriosus
Eisenmenger syndrome
Reversal of left-to-right shunt caused by elevated pulmonary arterial pressure exceeding systemic pressure
Helpful Clues for Less Common Diagnoses
Lymphadenopathy Associated with Infections
Most commonly seen with Histoplasma or Coccidioides infections
Primary M. tuberculosis usually unilateral disease
± miliary lung nodules
± lung consolidation
Low-attenuation lymph nodes common with endemic fungi
Elevated blood titers helpful in diagnosis
Lymphoma
Helpful Clues for Rare Diagnoses
Silicosis/Coal Worker’s Pneumoconiosis
Hilar and mediastinal nodal enlargement in 30-40%
Eggshell calcification of lymph nodes in 5%
Upper lobe predominant centrilobular or perilymphatic lung nodules
± calcification of lung nodules
Progressive massive fibrosis
Upper lobe conglomeration of nodules into large masses with volume loss and upward hilar retraction
Cavitation may indicate Tuberculosis superinfection
Berylliosis
Occupational lung disease
Ceramic industry, aerospace industry, nuclear power production
Identical radiographic appearance to sarcoidosis
Symmetric hilar and mediastinal lymphadenopathy
± lymph node calcification
Small nodules along fissures, subpleural lung, and bronchovascular bundles (perilymphatic distribution)
Positive BAL or serum beryllium lymphocyte proliferation test
Symptoms
Dyspnea most common
± cough, chest pain, and fatigue
Lymphadenopathy Secondary to Metastatic Disease
Unilateral hilar metastases are more common
Lymph nodes usually round and well defined
± central low density
Most common cause is bronchogenic carcinoma
Presence of contralateral hilar lymph node metastases indicates N3 disease (unresectable)
Angioimmunoblastic Lymphadenopathy
Erroneously called a systemic disease associated with immunodeficiency
Now accepted as peripheral T-cell lymphoma (non-Hodgkin lymphoma)
Mediastinal and hilar nodal enlargement ± lung disease
Pleural effusions in 40%
Amyloidosis
Hilar enlargement secondary to
Thickening of central airways from amyloid deposition
Lymph node enlargement
Perilymphatic lung nodules
± calcification in nodules and lymph nodes
Cardiac involvement leads to restrictive cardiomyopathy
Image Gallery
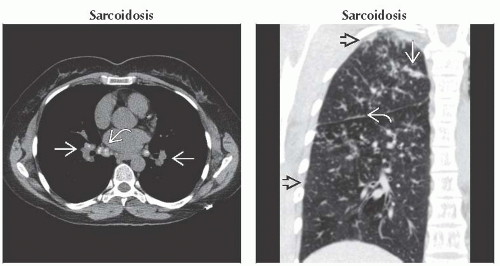 (Left) Axial NECT shows typical mildly calcified symmetric hilar
 and subcarinal and subcarinal  lymph nodes. Characteristic perilymphatic lung nodules are shown in the next image. (Right) Coronal NECT shows typical perilymphatic nodules in sarcoidosis. Note beading along the major fissure lymph nodes. Characteristic perilymphatic lung nodules are shown in the next image. (Right) Coronal NECT shows typical perilymphatic nodules in sarcoidosis. Note beading along the major fissure  , the subpleural nodules , the subpleural nodules  , and the airway nodules , and the airway nodules  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|