Chapter 36
Ventricular Tachycardia
1. What is the differential diagnosis of a wide complex tachycardia (WCT)?
The differential includes the following:
 Ventricular tachycardia (VT) (monomorphic or polymorphic)
Ventricular tachycardia (VT) (monomorphic or polymorphic)
 Supraventricular tachycardia (SVT) with aberrant conduction or underlying bundle branch block
Supraventricular tachycardia (SVT) with aberrant conduction or underlying bundle branch block
 Antidromic SVT using an accessory pathway for antegrade conduction (Wolff-Parkinson-White syndrome)
Antidromic SVT using an accessory pathway for antegrade conduction (Wolff-Parkinson-White syndrome)
 Toxicity related (hyperkalemia, digoxin, other drugs; Fig. 36-1)
Toxicity related (hyperkalemia, digoxin, other drugs; Fig. 36-1)
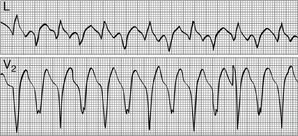
Figure 36-1 Bidirectional ventricular tachycardia in a patient with digitalis toxicity. (Modified from Marriott HJL, Conover MB: Advanced concepts in arrhythmias, ed 2, St Louis, 1989, Mosby.)
 Pacemaker-mediated tachycardia
Pacemaker-mediated tachycardia
2. What is the pathophysiologic substrate of VT?
3. What is the most common underlying heart disease predisposing to VT?
4. Can VT occur in other nonischemic heart diseases?
Scar-related VT can occur in other nonischemic conditions whenever an inflammatory or infiltrative disorder damages the myocardium. Sarcoidosis or Chagas disease are typical examples in which VT can occur as a result of such nonischemic scars. Fatty infiltration of the right ventricle leads to areas of unexcitable myocardium that can generate reentrant circuits in patients with arrhythmogenic right ventricular dysplasia. Myocardial scars leading to reentry also occur after surgical correction of congenital heart diseases. Dilated cardiomyopathies can lead to reentry within the diseased conduction system, the so-called bundle-branch reentry, where impulses use the right and left bundles as antegrade and retrograde pathways (less commonly in the opposite direction). Conceivably, any structural heart disease can lead to reentry.
5. Can VT occur in the absence of structural heart disease?
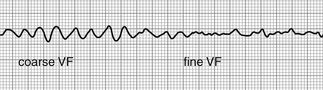
Primary electrical disorders can also lead to VT. Familial long QT syndromes typically lead to torsades des pointes, as does short QT syndrome. Brugada syndrome leads to primary ventricular fibrillation (Fig. 36-2). Catecholaminergic polymorphic ventricular tachycardia (CPVT) is the result of a mutation of the ryanodine receptor and typically causes exercise-induced bidirectional and polymorphic VT.