Chapter 18
St Segment Elevation Myocardial Infarction
1. What are the electrocardiograph (ECG) criteria for the diagnosis of ST segment elevation myocardial infarction (STEMI)?
 American College of Cardiology Foundation/American Heart Association (ACCF/AHA) criteria for STEMI consist of ST segment elevation greater than 0.1 mV (one small box) in at least two contiguous leads (e.g., leads III and aVF, or leads V2 and V3). The European Society of Cardiology (ESC) STEMI guidelines require 0.2 mV or greater ST elevation when analyzing leads V1 through V3 (but similarly, 0.1 mV elevation for other leads and/or territories). Figure 18.1 demonstrates the ECG finding of ST elevation in a patient with acute myocardial infarction.
American College of Cardiology Foundation/American Heart Association (ACCF/AHA) criteria for STEMI consist of ST segment elevation greater than 0.1 mV (one small box) in at least two contiguous leads (e.g., leads III and aVF, or leads V2 and V3). The European Society of Cardiology (ESC) STEMI guidelines require 0.2 mV or greater ST elevation when analyzing leads V1 through V3 (but similarly, 0.1 mV elevation for other leads and/or territories). Figure 18.1 demonstrates the ECG finding of ST elevation in a patient with acute myocardial infarction.
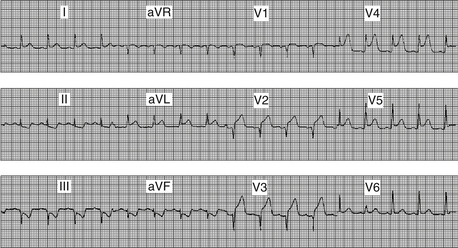
Figure 18-1 ST elevation in a patient with acute myocardial infarction (MI). There are 3 to 4 mm ST elevation in the anterior leads (V2 through V4), with lesser degrees of ST elevation in the lateral leads (I, aVL, V5, V6).
2. Is intracoronary thrombus common in STEMI?
Primary percutaneous coronary intervention (PCI) refers to the strategy of taking a patient who presents with STEMI directly to the cardiac catheterization laboratory to undergo mechanical revascularization using balloon angioplasty, coronary stents, aspiration thrombectomy, and other measures. Patients are not treated with thrombolytic therapy in the emergency room (or ambulance) but preferentially taken directly to the cardiac catheterization laboratory for primary PCI. Studies have demonstrated that primary PCI is superior to thrombolytic therapy when it can be performed in a timely manner by a skilled interventional cardiologist with a skilled and experienced catheterization laboratory team.
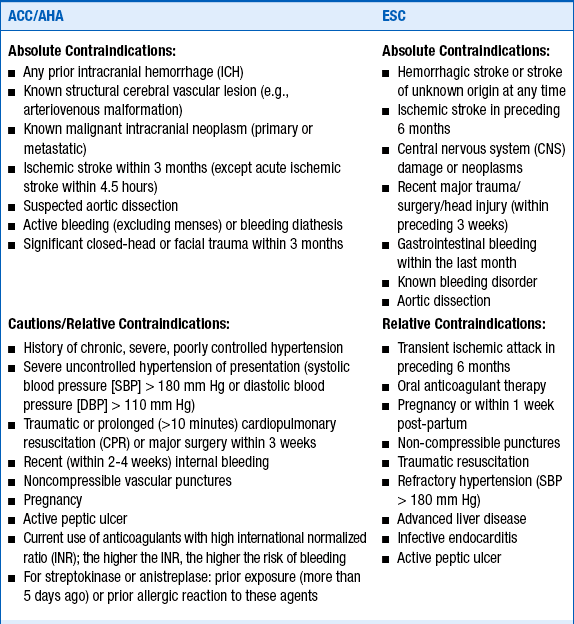
4. What are considered to be contraindications to thrombolytic therapy?
Several absolute contraindications to thrombolytic therapy and several relative contraindications (or cautions) must be considered in deciding whether to treat a patient with lytic agents. As would be expected, these are based on the risks and consequences of bleeding resulting from thrombolytic therapy. These contraindications and cautions are given in Box 18-1.
5. What is door-to-balloon time?
6. What is door-to-needle time?
7. In patients treated with thrombolytic therapy, how long should antithrombin therapy be continued?
Patients who are treated with unfractionated heparin (UFH) should be treated for 48 hours. Studies of low-molecular-weight heparins (EXTRACT, CREATE) and of direct thrombin inhibitors (OASIS-6) have suggested that patients treated with these agents should be treated throughout their hospitalizations, up to 8 days maximum. Guidelines for adjunctive antiplatelet and antithrombin therapy in patients treated with thrombolytic therapy are given in Table 18-1.
TABLE 18-1
2013 ACCF/AHA guidelines for adjunctive antithrombotic therapy to support reperfusion with fibrinolytic therapy
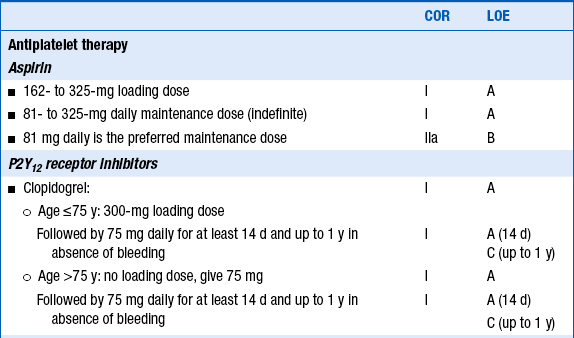
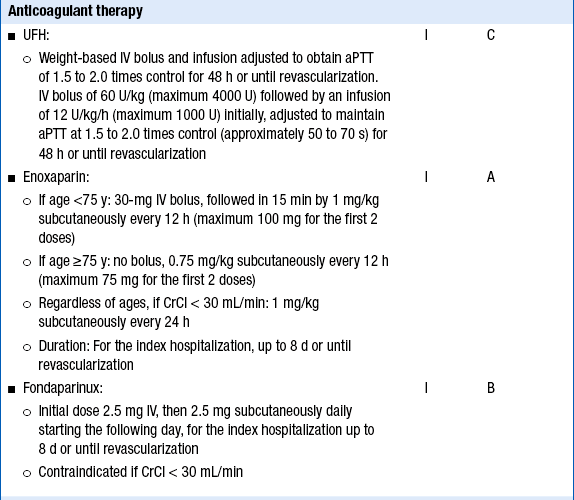
Reproduced with permission from O’Gara P, Kushner FG, Ascheim D, et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. J Am Coll Cardiol 2013;61(4):e78-e140.
8. Which patients with STEMI should undergo cardiac catheterization?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree