Chapter 54
Pericarditis, Pericardial Constriction, and Pericardial Tamponade
1. The pericardium is not necessary for life. What does it do? Why is it important?
2. What diseases affect the pericardium?
The pericardium is affected by virtually every category of disease (Box 54-1), including idiopathic, infectious, neoplastic, immune and inflammatory, metabolic, iatrogenic, traumatic, and congenital disease.
3. What is pericarditis? What are the clinical manifestations? What are the causes?
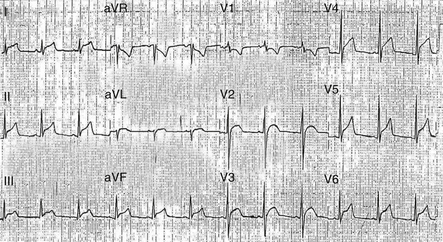
Acute pericarditis is a syndrome of pericardial inflammation characterized by typical chest pain (sharp, retrosternal pain that radiates to the trapezius ridge, often aggravated by lying down and relieved by sitting up), a pathognomonic pericardial friction rub (characterized as superficial, scratchy, crunchy, and evanescent), and specific electrocardiographic changes (diffuse ST-T wave changes (Fig. 54-1) with characteristic evolutionary changes and PR segment depression). Causes include infection (viral, bacterial, fungal, mycobacterial, or human immunodeficiency virus [HIV] associated), neoplasia (usually metastatic from lung or breast; melanoma, lymphoma, or acute leukemia), myocardial infarction, injury (postpericardiotomy and traumatic), radiation, myxedema, and connective tissue disease.
4. Should patients presenting with acute pericarditis be hospitalized? Why?
5. What is the treatment for acute pericarditis?
Acute pericarditis usually responds to oral nonsteroidal antiinflammatory drugs (NSAIDs), such as aspirin (650 mg every 3 to 4 hours) or ibuprofen (300-800 mg every 6 hours). Colchicine (1 mg/day) may be used to supplement the NSAIDs as it may reduce symptoms and decrease the rate of recurrences. Chest pain is usually alleviated in 1 to 2 days, and the friction rub and ST segment elevation resolve shortly thereafter. Most mild cases of idiopathic and viral pericarditis are adequately treated within a week or two of treatment start, but the duration of therapy is variable and patients should be treated until inflammation or an effusion, if present, has resolved. If colchicine is used, it should be given for 3 months; this is based on the randomized, open label Colchicine for Acute Pericarditis (COPE) trial. The intensity of therapy is dictated by the distress of the patient, and narcotics may be required for severe pain. Corticosteroids should be avoided unless there is a specific indication (such as connective tissue disease or uremic pericarditis) because they enhance viral multiplication and may result in recurrences when the dosage is tapered. Although the European Society of Cardiology (ESC) recently published guidelines for the diagnosis and management of pericardial diseases, there are only a few randomized, placebo-controlled trials from which appropriate therapy may be selected.
6. What is recurrent pericarditis? How is it treated?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree