Chapter 19
Cardiogenic Shock
2. What are the various types of shock?
3. Describe the clinical signs observed in cardiogenic shock and other types of shock?
The medical history and clinical examination help in making the diagnosis of cardiogenic shock. Feeling the extremities and examining the jugular veins provide vital clues: warm skin is suggestive of a vasogenic cause; cool, clammy skin reflects enhanced reflex sympathoadrenal discharge leading to cutaneous vasoconstriction, suggesting hypovolemia or cardiogenic shock. Distended jugular veins, rales, and an S3 gallop suggest a cardiogenic cause rather than hypovolemia. Figure 19-1 presents an algorithm for the evaluation and treatment of cardiogenic shock.
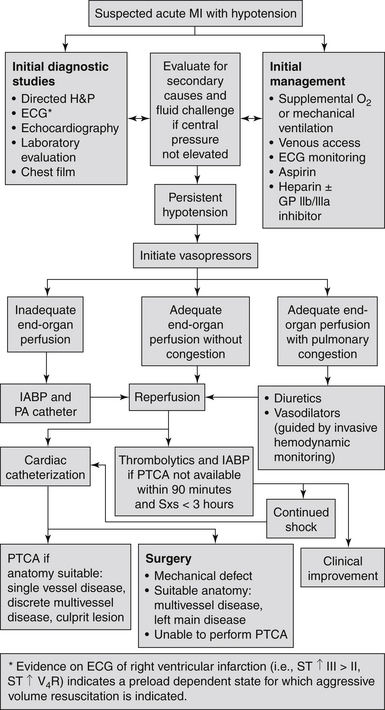
Figure 19-1 Evaluation and treatment algorithm for cardiogenic shock. (Modified from Hollenberg SM, Kavinsky CJ, Parillo JE: Cardiogenic shock. Ann Intern Med 131:47-59, 1999.) ECG, Electrocardiogram; GP, glycoprotein; H&P, history and physical examination; IABP, intraaortic balloon pump; MI, myocardial infarction; PA, pulmonary artery; PTCA, percutaneous transluminal coronary angioplasty; Sxs, symptoms.
4. Do all patients with cardiogenic shock have an increased heart rate?
5. What are the determinants of central venous pressure (CVP)?
The normal CVP is 5 to 12 cm H2O. Intravascular volume, intrathoracic pressure, right ventricular function, and venous tone all affect the CVP. To reduce variability caused by intrathoracic pressure, CVP should be measured at the end of expiration.
6. What is the significance of a loud holosystolic murmur in a patient with shock after acute myocardial infarction?
7. How can one differentiate cardiogenic from septic shock?
8. What is the most common cause of cardiogenic shock?
9. Describe the pathophysiology of cardiogenic shock among patients with acute myocardial infarction?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


