Chapter 30
Aortic Valve Disease
1. What is the most common cause of aortic stenosis (AS) in developed countries today, and what is the current thinking about its pathogenesis?
Although rheumatic fever was once the most common cause of AS, today calcific disease of either bicuspid or tricuspid AS is the leading cause. Once considered a degenerative disease, it is now clear that calcific AS is an inflammatory process with many similarities to atherosclerosis. A normal aortic valve, and AS as a result of congenital bicuspid aortic valve, rheumatic AS, and calcific AS, are shown in Figure 30-1.
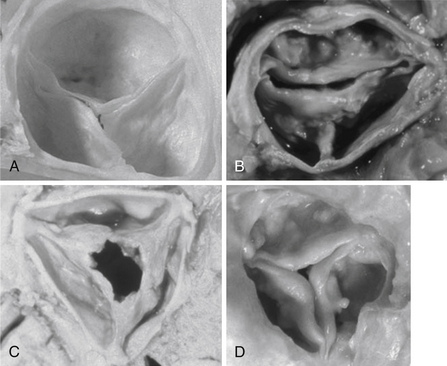
Figure 30-1 Normal and stenotic aortic valves. A, Normal aortic valve. B, Congenital bicuspid aortic stenosis. A false raphe is present at 6 o’clock. C, Rheumatic aortic stenosis. The commissures are fused with a fixed central orifice. D, Calcific degenerative aortic stenosis. (From Libby P, Bonow RO, Mann DL, Zipes DP: Braunwald’s heart disease: a textbook of cardiovascular medicine, ed 8, Philadelphia, 2008, Saunders.)
2. What is the pathophysiology of AS, and what effect does it have on the left ventricle (LV)?
AS exerts a pressure overload on the LV. Normally, pressure in the LV and aorta are similar during systole, as the normal aortic valve permits free flow of blood from LV to aorta. However, in AS, the stenotic valve forces the LV to generate higher pressure to drive blood through the stenosis, causing a pressure difference (gradient) from LV to aorta. The LV compensates for this pressure overload by increasing its mass (left ventricular hypertrophy [LVH]). The ways in which the transvalvular gradient are measured and quantified are shown in Figure 30-2.
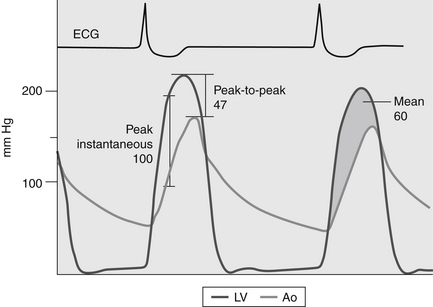
Figure 30-2 Various methods of describing an aortic transvalvular gradient. The figure shows representative pressure tracings measured during cardiac catheterization in a patient with aortic stenosis. One pressure transducer is placed in the left ventricle and a second pressure transducer is positioned in the ascending aorta. The peak-to-peak gradient (47 mm Hg) is the difference between the maximal pressure in the aorta (Ao) and the maximal left ventricle (LV) pressure. The peak instantaneous gradient (100 mm Hg) is the maximal pressure difference between the Ao and LV when the pressures are measured in the same moment (usually during early systole). The mean gradient (shaded area) is the integral of the pressure difference between the LV and Ao during systole (60 mm Hg). (From Bashore TM: Invasive cardiology: principles and techniques, Philadelphia, 1990, BC Decker, p. 258.) ECG, Electrocardiogram.
3. How is left ventricular hypertrophy compensatory?
The Law of Laplace states that systolic wall stress (σ) is equal to:
4. Are there downsides to LVH?
5. What are the classic symptoms of AS, and why are they important?
The classic symptoms of AS are angina and syncope and those of heart failure (dyspnea, orthopnea, paroxysmal nocturnal dyspnea, edema, etc.). Their importance is graphically displayed in Figure 30-3. In the absence of symptoms, survival is nearly the same as that of an unaffected population. However, at the onset of symptoms there is a dramatic demarcation such that mortality increases to 2% per month, so that three-quarters of all AS patients are dead within 3 years of symptom onset unless proper therapy is instituted. It should be noted that when the data for this figure were compiled, the etiology of AS was usually rheumatic or congenital heart disease and the average age of the patients was 48 years. Since then the etiology of AS has changed (as noted above) and with it the age at symptom onset has increased by about 15 years.
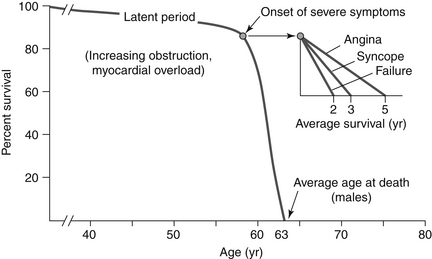
Figure 30-3 The natural history of medically treated aortic stenosis. Once symptoms develop in a patient with aortic stenosis, the average survival with medical treatment (e.g., no curative surgery) is only 2 to 5 years. (From Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL: Sabiston textbook of surgery: the biological basis of modern surgical practice, ed 18, Philadelphia, 2008, Saunders.)
6. What are findings of AS on physical examination?
7. How is echocardiography used to assess the patient with AS?
as the valve area decreases, velocity of flow must increase for flow to remain constant (Fig. 30-4). This increase in blood velocity at the valve orifice is detected by Doppler ultrasound. The severity of AS is assessed using the factors given in Table 30-1. In general, if a patient has the symptoms of AS and assessment indicates severe disease, then the symptoms are attributed to AS. However, it must be emphasized that the benchmarks listed here are only guidelines to severity, and some patients exhibit exceptions to them.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree